Covid-19 (obsolete)
aka SARS-CoV-2, 2019-nCoV, Wuhan pneumonia, Coronavirus
Re-write
This essay has grown out of control so I have decided to re-write much of it.
Rather than discard the whole thing I have decided to retain the old version. The new version can be found here.
TL;DR
Don’t Panic!
Yes, that’s it. That’s the summary.
OK. Here’s why (for England and Wales unless otherwise stated):
- The high numbers of deaths in April and May 2020 were preceeded by a 2 year period of exceptionally low numbers of deaths. We can assume that many of those who died had survived longer than would normally be expected.
- The lockdown from 23 March seems to have had an immediate negative effect followed by a later, lesser positive effect on death numbers.
- Changes to lockdown rules such as the re-opening of pubs and restaurants and the imposition of mask-wearing have had no effect on death numbers.
- The majority of those who have died with Coronavirus were elderly or had underlying poor health conditions - which is what we see among those who die in normal times. The ratio of ‘elderly’ to other age groups dying during the peak is the same as in normal times.
- The ratio of men:women dying during the peak is the same as in normal times. In normal times men die younger than women.
- From week 24 of 2020 (mid June): It’s over. Yes, people are still catching the bug and dying from it - but they’re not catching or dying of ‘flu in the numbers we would expect at this time of year. It doesn’t matter if you die of Coronavirus instead of ‘flu.
- All-cause deaths are down on the trend average from this time on.
- As at week 44 (latest weekly figures from ONS) there is no sign of a so-called ‘second wave’ in all-cause death numbers.
- Despite this Wales and then England have started further national lockdowns in late October/early November.
(For those who don’t recognise what TL;DR means - it either means Too Long; Didn’t Read, or Too Long; Don’t Read depending on the context. If you think of yourself as an executive - perhaps with too little time or a short attention span - you could take it to mean Executive Summary.)
Just how bad is it?

It was bad but we’ve had worse in recent times.
*Notes:
- The majority of the data is drawn from Office of National Statistics (ONS) Excess Winter Mortality datasets for England and Wales combined with their population estimates and population projections (blue columns).
- I predicted that ONS would not use their usual calculation when they reported the Excess Winter Deaths for the 2019-2020 season. They excluded any deaths where Coronavirus was mentioned on the death certificate when calculating the non-Winter baseline.
- The calculations I have used to estimate recent excess deaths (red/yellow column only) are mine - don’t blame ONS if I have made invalid assumptions in the calculation. I have calculated that in weeks 11 to 28 (about 4 months) there were 60,083 more deaths than the 2014-2018 five year average.
- Data for the Covid-19 (red) column is drawn from the ONS weekly dataset count of deaths registered in the four months since week 11 (beginning 7 March) of 2020 to week 28 (ending 10 July) in England and Wales which mention Covid-19 on the death certificate.
- The ‘lockdown’ (yellow) column is the difference between the cumulative excess deaths since week 11 and the Covid-19 column. As such it represents deaths which are not explained by the Covid bug.
- As at 12 August UK government agencies reckon that 41,329 people have died from Covid-19 in the whole of the UK - revised down from 46,706 due to a recent change in the way Public Health England (PHE) counts Covid-19 deaths.
There have been 50,505 deaths in England and Wales where Covid-19 was mentioned on the death certificate in the four months since such deaths were first recorded. This just exceeds the excess Winter deaths of 2017/2018 when there were 49,410 excess death registrations in the four months from the beginning of December 2017 in England and Wales. The figures show 2017/2018 was quite a bad ‘flu season (highest absolute number of excess Winter deaths since 1975/1976) but I certainly don’t recall any media panic - at least not until after it was over. When we express the excess deaths as a percentage of the population at the time, Covid-19 is the 31st worst 4-month peak in the last 70 years in England and Wales. To avoid any misunderstanding note that I am comparing a 4-month peak above the 5 year average for the same time of year (Covid-19, mid-March to mid-July) against 4-month peaks above the rest of the corresponding year (excess Winter deaths, December-March above August-November and April-July). Excess Winter deaths are normal and expected - Covid-19 was unusual.
| Rank | Season | % of pop | # deaths |
|---|---|---|---|
| 32 | 2017/2018 | 0.0844% | 49,410 |
| 31 | Covid | 0.0852% | 50,505 |
| 30 | 1981/1982 | 0.0854% | 42,380 |
| 29 | 1982/1983 | 0.0863% | 42,820 |
| 28 | 1964/1965 | 0.0885% | 41,730 |
| 27 | 1959/1960 | 0.0902% | 41,060 |
| 26 | 1998/1999 | 0.0907% | 46,810 |
| 25 | 1996/1997 | 0.0929% | 47,700 |
| 24 | 1999/2000 | 0.0935% | 48,420 |
| 23 | 1989/1990 | 0.0938% | 47,200 |
| 22 | 1971/1972 | 0.0944% | 46,270 |
| 21 | 1972/1973 | 0.0947% | 46,630 |
| 20 | 1984/1985 | 0.0954% | 47,380 |
| 19 | 1978/1979 | 0.0981% | 48,490 |
| 18 | 1985/1986 | 0.0991% | 49,330 |
| 17 | 1951/1952 | 0.1027% | 44,950 |
| 16 | 1968/1969 | 0.1046% | 50,630 |
| 15 | 1963/1964 | 0.1057% | 49,510 |
| 14 | 1953/1954 | 0.1069% | 47,180 |
| 13 | 1975/1976 | 0.1175% | 58,100 |
| 12 | 1965/1966 | 0.1202% | 57,120 |
| 11 | 1957/1958 | 0.1284% | 57,780 |
| 10 | 1969/1970 | 0.1394% | 67,790 |
| 9 | 1954/1955 | 0.1458% | 64,670 |
| 8 | 1967/1968 | 0.1460% | 70,260 |
| 7 | 1961/1962 | 0.1492% | 68,820 |
| 6 | 1960/1961 | 0.1504% | 68,880 |
| 5 | 1955/1956 | 0.1515% | 67,560 |
| 4 | 1958/1959 | 0.1721% | 77,920 |
| 3 | 1952/1953 | 0.1883% | 82,670 |
| 2 | 1962/1963 | 0.1929% | 89,600 |
| 1 | 1950/1951 | 0.2441% | 106,400 |
Contents
- aka SARS-CoV-2, 2019-nCoV, Wuhan pneumonia, Coronavirus
- Re-write
- TL;DR
- Just how bad is it?
- Contents
- Introduction
- What is it?
- Where did it come from?
- How did it spread so fast?
- Methodology
- An alternative view
- A rose by any other name… terminology matters.
- It’s a very deadly plague…
- Counting the victims
- Is COVID-19 targeting…
- A coat of motley
- Resistance is futile!
- The drugs don’t work
- Vaccination and inoculation
- Drastic action… We mustn’t panic!!
- Tests, tests and more tests
- Testing technology
- Restrictions - Erosion of liberty.
- Community transmission
- Masks
- Education qualifications
- How do we get out of lockdown?
- The second wave - or ‘Winter’s coming’
- Emperor’s new clothes? Boy who cried ‘wolf!’.
- The economic impact
- ‘Did’, ‘Probably did’, ‘Possibly did’, ‘Could have’, ‘Might have’, ‘Didn’t’…
- ‘Cases’ vs deaths
- What will history say?
- From the department of Egregious Statistics and Applied Flannel at the University of West Fantasia
Introduction
At the risk of getting my head shot off I’ll stick it above the parapet as I have very strong opinions and objections about much of the coverage about ‘the bug’.
I am not a virologist or epidemiologist or statistician or journalist so feel free to disagree with me - or preferably educate me! I have no regular following on this blog (I don’t write regularly anyway) so my opinions are unlikely to cause any ripples in public policy.
Some people may find some of the following brutal or even offensive but I have no intention to offend anyone. If you are offended, please do take the time to explain to me why. It may be that I have been clumsy in my choice of words, or may be using ‘gallows humour’ or that I am just plain wrong - or we may just have to disagree.
Let’s not set off on the wrong foot; it’s a nasty bug. Its spreading and some people (potentially me and/or people I know and love) will die of it.
Yes, I know bug is strictly a technical term for a type of insect with piercing mouthparts but most people recognise the term to loosely describe anything which infects another host - whether we’re talking about multi-cellular parasites (think gut worms), or single cell bacteria (typhoid, cholera) or viruses (Ebola, chickenpox or SARS-CoV-2). Another commonly used word for this sort of thing is ‘germ’.
With that out of the way let’s look at it in a little more detail.
What is it?
Coronavirus disease 2019 is caused by a virus. The virus can be transmitted from person to person. Its main symptoms are said to be fever (raised body temperature) and a persistent dry cough. In severe cases the sufferer may develop pneumonitis (viral pneumonia, inflammation of the lining of the lungs) and require treatment in hospital to recover. Some sufferers will die because of it - either from its direct effects or because the infection exacerbates a preexisting condition (for example, physical or psychological stress triggering heart attacks).
The virus is a coronavirus - there are many different types or strains of coronavirus. Coronaviruses are so named because of the appearance of the virus particles under very powerful microscopes - they look like they’re spiky crowns. Corona=crown. Their appearance has nothing much to do with their genetic make up or relationship to other viruses. Because of the coverage in the media the virus causing Covid-19 is now widely known as ‘Coronavirus’ with a capital ‘C’.
About 10% of common colds are caused by coronaviruses too (no, probably not this bug). Most of the rest are caused by rhinoviruses. Rhinoviruses are so-called because they affect the nasal passages and can cause a runny nose. Rhino=nose. Yes, rhinoviruses are named because of how the body reacts to them - not for how they look. Again it says nothing about their genetics or relationship with other viruses.
The SARS virus of 2003 and the MERS virus of 2012 are also both coronaviruses. The ‘RS’ part of their names stands for ‘Respiratory Syndrome’ - ie they’re named for what they do to us.
Where did it come from?
A common theory is that it is a zoonosis - an infectious agent which has crossed from animal species to humans and then spread from person to person. It has been suggested that the virus may have jumped the species barrier via live animals being sold at a food market in the city of Wuhan in Hubei province, China.
There is much unhelpful speculation about the source of the current pandemic; a young child I know was taught something about the virus at school and reported back to his parents that ‘Someone in China ate an infected snake and then coughed on a bat which then coughed on loads of other people’. All very amusing until you realise that the child now thinks that ‘the Chinese people are to blame because they eat weird stuff like snakes’. Xenophobia can lead to racism. I don’t want to suggest that was what the child was taught - but it is what they learned.
One thing the above story does highlight is that infectious agents can be transmitted from animals to people and back again. Tuberculosis (TB) is an example of a disease which is known to spread from cattle to people and vice-versa.
What the above story does not do is help to explain in any way why we have a pandemic now. Was this the first time a person ever ate a snake? (No.) Or the first time someone ever coughed on a bat? (No.) Or the first time a bat coughed on people? (No.) So what changed? The answer is simple but also complicated: the bug evolved. In other words it changed in such a way that it became more ‘successful’ in getting itself replicated in people. Having changed (mutated) and spread we now find it nearly everywhere in the world - like the common cold in that respect.
How did it spread so fast?
So having apparently started in Wuhan in December 2019 (bear with me), how did it reach the Heir to the Throne of the United Kingdom and the Prime Minister of Canada’s household and many other people around the world in March 2020? The answer is of course, person-to-person transmission - and that it did not ‘start’ in December 2019. It seems that like most successful viruses it can be passed on before any significant symptoms (like fever, persistent coughing or death) appear. Indeed, few things limit the success of bugs more than a very high kill rate or very early symptoms. If a bug quickly kills off all its hosts it will have nothing left to spread to and it will therefore not be successful - but that’s not great news for the hosts though.
The bug was first discovered to be a new strain of coronavirus circulating in Wuhan in December 2019. It had probably been quietly spreading for a few months prior to that and it was only after a change in health monitoring data was noticed that scientists started looking for it. Instead of spreading worldwide in just 4 months it had almost certainly been going on for 6 months or more, and quite possibly a whole year.
Italian researchers have also now spotted a change in their health monitoring data for the last quarter of 2019. At the time of writing this post they are investigating to see if these might be Covid-19 cases. If these do prove to be Covid-19 then this will prove that the bug has been circulating since well before its discovery in December 2019. It will also throw open the debate about where it came from; maybe the bug originated in Italy and not China. Who knows? I was tempted to ask ‘Who cares?’ but it is important to find out so that we can make decisions based on solid facts.
Initially, and simplistically, the spread of infections in general can be described as a mathematical ‘geometric progression’. The maths involved is actually quite simple:
Imagine a FICTIONAL bug where each infected person infects 3 more people each day (replication rate=3 per day), then the infection spreads as shown in the table and graph below. IMPORTANT: this is an example of the maths - not what Covid-19 or any real bug could actually do.
| Day | New | Running |
|---|---|---|
| infections | total | |
| 1 | 1 | 1 |
| 2 | 1x3=3 | 1+3=4 |
| 3 | 4x3=12 | 4+12=16 |
| 4 | 16x3=48 | 16+48=64 |
| 5 | 64x3=192 | 64+192=256 |
| 6 | 256x3=768 | 256+768=1,024 |
| 7 | 3,072 | 4,096 |
| 8 | 12,288 | 16,384 |
| 9 | 49,152 | 65,536 |
| 10 | 196,608 | 262,144 |
| 11 | 786,432 | 1,048,576 |
| 12 | 3,145,728 | 4,194,304 |
| 13 | 12,582,912 | 16,777,216 |
| 14 | 50,331,648 | 67,108,864 |
| 15 | 201,326,592 | 268,435,456 |
| 16 | 805,306,368 | 1,073,741,824 |
| 17 | 3,221,225,472 | 4,294,967,296 |
| 18 | 12,884,901,888 | 17,179,869,184 |

Before the end of day 18 everyone in the world (about 8 billion people) would be infected in this FICTIONAL example.
Of course, the initial geometric progression would actually be limited by a number of different effects:
- How soon after becoming infected does a person become infectious (next day in our FICTIONAL example)?
- How many un-infected people remain to become infected? Such a rate limiting effect would cut in well before most people are infected. If half the people on an isolated island were infected then they could not pass on the infection to more than the other half so the local replication rate would fall to one for that day and zero for the following day.
- What proportion of infected people die or recover, and after how many days?
- Whether or not recovered people have immunity to reinfection?
For our FICTIONAL bug if each infected person only infects 2 new people each day (replication rate=2 per day) then it doesn’t take much longer to reach the whole population - just 22 days.
If each infected person only infects one other per day (replication rate=1 per day) then it takes all of 34 days to infect everyone.
If there’s only a 50:50 chance of an infected person infecting someone else each day (replication rate=0.5 per day) then it would take 58 days to spread around the world.
The shape of the graph in each example is near enough identical - the only difference is the number of days it takes to reach the world population limit of 8 billion. Do bear in mind though that all these graphs start with 1 infected at the beginning of day 1 - the arithmetic has been building up throughout and only really shows up on the scale of the graph in the last few days.

Back closer to the real world… At the time of writing (atToW) about 1 million people have been diagnosed with Covid-19. If the first infection was 180 days ago (6 months) then if each infected person had an 8% chance (odds of 25:2 against) of infecting one other person per day (and none recovered or died) then we would have easily reached this total - and because 1 million is so few people compared with the world’s population (or even the Chinese province of Hubei’s population, 58 million people) the rate limiting step of lack of new people to infect has not even started to become relevant.
Geometric progressions can build up fast. Infections seem to start in this way (this is why we say that ideas or jokes that spread rapidly - eg on the Internet - have ‘gone viral’) before other effects start limiting them. This limiting is what happens in the real world. Basically, geometric progressions can only be applied at the start of an epidemic or pandemic - which is where we were when I started writing this post.
Any reporter or so-called ‘Expert’ who uses the term ‘exponential’ to describe the spread of the Covid-19 or any other bug should be ignored or laughed at (unless they say ‘not exponential’). No bug has ever, ever spread exponentially.
| BBC news reported on 2 Oct 2020: | |
|---|---|
| Sage, the body which advises the UK government, say it is still “highly likely” the epidemic is growing exponentially across the country. |
Oh dear.
We don’t know how many people are actually infected with the Covid-19 bug. We can’t test 8 billion people (the whole world). It would take too long and cost too much to produce, use and process 8 billion test kits and by the time we had done so, anyone who had tested negative might well have caught the bug and need retesting. We mostly only test those who have the known symptoms of the disease and in many cases only those whose condition requires hospital treatment. Guess, what? If we only test people who we think are sick then we should not be surprised if a high proportion of the tests come back positive. It tells us nothing about the people we have not tested or therefore how widespread the bug actually is. Worse than that, only testing very sick people means we get a distorted view of how dangerous the bug is - everyone who tests positive is really unwell - but that’s because we only test people who are really unwell. This effect is called ‘selection bias’ and is a statistician’s sin.
If, as with most other communicable diseases, people become infectious before they have symptoms then the bug will continue to be spread through our population despite our best efforts. Epidemiologists use mathematical models (far more refined than simple geometric progressions) to try to work out how many people might be infected at any time - but these models have to be based on some understanding of how the bug is behaving - and how people are behaving too. In a fairly recent announcement the UK chief medical adviser to the government estimated that the actual number of infected people in the UK might be between 8 and 16 times the number of formally tested/diagnosed folk but gave no details of the basis for this estimate. Well, you’ve got to say something when your bosses try to pin you down. The point is that it is crucially important to gather data about this bug. Gathering data is not ‘doing nothing’.
It is widely reported that the UK government’s Covid-19 strategy of ‘lockdown’ and ‘social distancing’ is informed by a mathematical model developed by a team at Imperial College London led by Professor Neil Ferguson. This will not be their only source of advice. Indeed, they’re probably getting more conflicting advice than they can deal with.
Rather interestingly Iceland has been investing in much more testing than most countries. They only have a population of about 0.3 million and they seem to have been trying to test a random cross section of their people and (atToW) have found just over 1,000 positive cases with 25 seriously ill and 2 deaths so far out of around 15,000 tests completed. Unfortunately they’re running out of test kits so they now have to slow down the testing. It’s early days yet, but their death rate stats look better than most other countries. In addition it appears that Iceland’s testing of people without symptoms may have revealed that 50% of infected people experience no symptoms at all. There may be what statisticians call ‘confounding factors’ (unusual population, hidden selection bias, poor methodology - whatever) or it might be real. If that result is real then there are a number of implications:
- It’s more contagious than we thought or it’s been going around undetected for longer than we thought.
- There are many more infected people out there than we thought so more people will catch it.
- You may be infected and not know it - so you may be spreading it.
- A much lower percentage have severe symptoms than we thought.
- The death rate is much lower than we thought (OK that’s effectively a repeat of the above point; death is defintely a very severe symptom).
Watch this space - with hope.
Methodology
To try and understand the impact of Covid-19 we have to compare data that have been gathered in ‘normal times’ with recent data. Obviously there’s no point trying to compare ‘number of Covid-19 cases’ with the same period last year as the bug was only identified in December 2019. We might try to compare how many available beds there are in our hospitals in week 12 2020 with week 12 2019 - but that might provide a misleading reassurance because NHS England (for example) have been following a deliberate policy of delaying hospital admissions for ‘routine’ care to ensure they have capacity if (when?) there’s a large increase in Covid-19 cases.
But just what is a ‘case’ of Covid-19? It seems a silly question to ask but the ‘D’ in ‘CoViD-19’ stands for ‘disease’. Media reports seem to use the term ‘case’ interchangably with ‘tested positive’. Just like with almost any other bug you can be infected and not experience any sign of disease or have it on the surface of your tonsils and not even be infected. Is that a ‘case’ of Coronavirus Disease 2019? No, it isn’t - but it is useful science.
Even the ONS approach of including for comparison numbers of deaths averaged over the previous 5 years is flawed - though it has the advantage of being simple to calculate. The age distribution and size of the population is not static over time. For example in 2020 there is a spike in the number of people aged 70-75 (the so-called ‘baby boomers’ - people born soon after the end of WWII). The sizes of the different agegroups are influenced by the original birthrates, immigration, emigration and death rates since birth. If we want to compare numbers of people in different agegroups dying with data from previous years we need to take these changes into consideration. We need to work out the rate or percentage of each agegroup that is dying in any given period. Fortunately ONS publishes population estimates and projections which we can incorporate with their death registration data to calculate the rates of deaths over time.


I have chosen to compare the rate of deaths from all causes and deaths due to ‘Diseases of the respiratory system’ registered in England and Wales as these data are gathered and published on a weekly basis by the ONS, and the datasets covering the past ten years are readily available. Rather than use ONS’ provided 5 year average based on actual numbers of people dying, I have used a ten year (2010-19) average of rates of people dying. I believe these figures are accurate and self contained (ie I don’t need to combine information from other agencies which may not use compatible methods). I see no particular reason to think that the progress of the epidemic in England and Wales will be significantly different than anywhere else**. I do recognise that using deaths as a measure of the severity of the epidemic can be misleading:
- It does not measure how much effort (and success) is going into preventing deaths attributed to this bug.
- Death is the most extreme endpoint, the vast majority of people who catch this bug will not die because of it.
- Because death is an endpoint, it does not measure how many are currently suffering with or have recovered from the bug.
- It gives no measure of how many suffer long-term health damage as a result of the infection.
- Using registered deaths as our measure introduces further delays. Deaths are usually registered within 5 days of the event, but under some circumstances (especially including public holidays) registration can be delayed beyond that. ONS produce their reports 11 days after the Friday of each week.
To quote Groucho Marx: ‘Die, my dear? Why that’s the last thing I’ll do!’
The UK government has set up a ‘dashboard’ website showing various metrics about the progress of the epidemic in the UK. It details number of tests done per day, number of new ‘cases’ (see below) per day, number of people admitted to hospital (or to ICU) as a result of Covid and number of new deaths per day. It is fundamentally flawed because it gives no context or baseline for any of the figures (it’s not an increase if numbers of deaths are up 5% if the size of the population has also increased by 5%):
- Tests: The numbers include ‘Pillar 1’ and ‘Pillar 2’ tests but no corresponding results. The introduction of ‘Pillar 2’ tests part way through the epidemic seems to correspond to a sudden increase in ‘cases’ which suggests the methodology of the two ‘pillars’ is not comparable.
- Cases: Much alarm has been voiced in the media over the sharp increase in ‘cases’ since mid-July. The observed increase corresponds to the introduction and increasing numbers of ‘Pillar 2’ testing in England and Wales.
- The increase in positive results seems roughly proprtional to the increasing ratio of Pillar 2:Pillar 1 tests.
- Despite the sharp increase in ‘cases’ from mid-July there is no increase in hospital and ICU admissions until September - and then it is a gradual increase. If these observations are related at all then Covid-19 has changed from a disease with an onset of less than a week to an onset of about 6 weeks - which is not credible.
- Health: There has been a slight increase in hospital and ICU admissions since the beginning of September as compared with mid-July - there is no corresponding data shown for admissions for ‘normal times’ (ie how many ICU ventilator beds were occupied at this time of year in 2019 and previous years?).
- Deaths: There has been an increase in deaths attributed to Covid-19 since the beginning of September as compared with mid-July. A few problems here:
- In mid-August PHE revised their count of deaths down by more than 5,000 from 46,706 to 41,329 (a reduction of 12%). ONS publish death figures that are more consistent (they can’t be retrospectively changed by a change in definition of ‘a Covid death’) but the numbers are subject to greater delay in reporting.
- The increase in Covid-19 deaths corresponds to a decrease in reported deaths from respiratory diseases (in week 37 respiratory deaths are 14% below the 5-year average). It really does not matter whether someone has died with Covid-19 or pneumonia caused by some other bug. What would matter is an overall increase or decrease in death rate - and that is not shown on the dashboard.
- All cause deaths rates have barely increased compared with 10-year averages.
We can compare death rates week by week between years and even average the data to try to account for particularly good or bad seasons. Using this approach certainly shows the Covid-19 bug to have killed a lot of people mid-March to mid-May - but continuing the same analysis approach shows that the epidemic has run its course in England and Wales. Sure, some people will still die of the bug; but if they do, they won’t die of ‘flu.
I intend to update all the relevant charts in this post as new data is published by ONS. This may result in a mis-match between the text and the charts - in which case the chart will be more up-to-date and I’ll (eventually, maybe) get around to editing or re-writing the text.
| ONS | Week | Registrations | Published |
|---|---|---|---|
| Dataset | up to | ||
| Current | 50 | 11 Dec | 22 Dec |
| Next | 51 | 18 Dec | 30 Dec |
**It appears that the progress of the disease in England is slightly different to other countries of the UK and elsewhere in Europe. No other country which contributes mortality statistics to EuroMOMO shows a spike in numbers of deaths among the 15-44 agegroup corresponding to the pandemic. EuroMOMO gathers and publishes weekly mortality statistics from Austria, Belgium, Denmark, Estonia, Finland, France, Germany (two regions: Hesse and Berlin), Greece, Hungary, Ireland, Italy, Luxembourg, Malta, Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, UK (all four regions: England, Northern Ireland, Scotland and Wales). Of all these countries, only UK England shows statistically significant excess deaths among 15-44 year olds. Furthermore Austria, Denmark, Estonia, Finland, Germany (the two regions), Greece, Hungary, Luxembourg, Malta, Norway and Portugal show almost no significant increase in mortality at all across all age groups during the pandemic. Have they actually defeated or escaped the bug or perhaps just delayed the inevitable? Are these differences between these and more badly affected countries a matter of extent and timing of lockdown policy and obedience, performance of health or social care, climate and environment, wealth or age or ethnic or genetic distribution or density of the population? We won’t know until it’s over.
An alternative view
One accepted way of looking at the course of the epidemic in England and Wales is to focus on the number of deaths as compared with ‘normal times’. Without doubt, there were far more deaths registered in weeks 14-21 of 2020 than in those same weeks in any recent year. However, if we look at the rate of deaths per week for each age group (eg what pecentage of those aged 85+, 75-84, 65-74 etc died each week) starting from as far back as January 2010 (the earliest I could find) and calculate the rolling 52 week (~1 year) averages (to smooth out seasonal ‘bumps’) we can then see a remarkable repeating pattern: periods of low rates of deaths are followed by periods of higher rates with an almost completely flat trend line. What we then notice however is that for about a year from early 2019, 52-week average death rates were considerably below the trend line for the top three age groups. This means deaths were below trend for about two years among these groups…

From the graph we can see that the 10-year trend in deaths of the 85+ agegroup is about 0.28% of the population per week (ie around 14.5% of people aged 85+ die each year - or more optimistically, 85.5% survive). This is normal. The rate trends for all of the age groups can be derived from the data and are roughly:
| Agegroup | Average weekly | Average annual |
|---|---|---|
| death rate | equivalent death rate | |
| Under 1 | 0.0078% | 0.41% |
| Age 1-14 | 0.0002% | 0.01% |
| Age 15-44 | 0.0013% | 0.07% |
| Age 45-64 | 0.0082% | 0.43% |
| Age 65-74 | 0.0297% | 1.54% |
| Age 75-84 | 0.0864% | 4.49% |
| Age 85+ | 0.2841% | 14.77% |
We know that there are seasonal variations on these average rates (higher in Winter, lower in Summer) which we can show on a chart*.

* Note that seasonal effects almost completely disappear below the top three age groups (ie under 65 years). Note also the effect on the death registrations of the fixed public holidays in weeks 22, 35 and at the beginning and end of the year. The more variable Easter and Mayday holidays produce less well defined dips.
Combining the underlying and seasonal rates and multiplying by the number of people in the relevant population subset allows us to produce a calculated normal number of deaths for each week from Jan 2010 to date with which we can compare the actual number of deaths registered*.

A feature of this analysis is that it allows us to quantify the numbers of deaths below and above the calculated normal for each week. When we do this we find that over the ~2 years from early 2018 (week 17 2018) to early 2020 (week 11 2020) there were about 39,300 (~3.8%) fewer deaths than would be expected. (*The colourful shading is to show the basis on which ONS calculates excess Winter mortality, they average the Autumn and following Spring and compare that with the Winter - as you can see the majority of the epidemic occurred in Spring 2020 which will affect how ONS reports the EWM for Winter 2020).
So what’s the alternative view? It’s not that the bug cut short so many lives; it’s that 39,300 people had lived rather longer than expected - and then the Covid-19 epidemic arrived.
Don’t get me wrong: When you consider that most of those 39,300 people died in a period of just 8 weeks, that’s an awful lot of people. But spread out over the previous 2 years we would not have noticed those deaths unless personally involved.
The result is that we no longer have a large population of frail people who we might have expected to die by now - and so the all-cause death rate (including those from the Covid bug) has fallen to normal for the time of year (actually weeks 22-42 tracking a little below trend). .
Remember: these numbers and charts are for England and Wales only. It will be interesting to see how other countries have fared over the last ten or so years.
If you want to look at another country’s data a good source is https://www.mortality.org/. For England and Wales they take the ONS provided mortality and population data and aggregate it into broader agegroups so it can be compared more easily with data from other countries and years (FYI the death rates they quote are yearly fraction equivalent - ie if they give a death rate of 0.14 for a particular population in a given week then if that rate was sustained for a whole year 14% of the relevant population would die).
A rose by any other name… terminology matters.
Epidemic, Pandemic or Endemic or just Seasonal? Infection or ‘case’?
This is a bit geeky but I think it’s worth an attempt to explain the difference between these slightly technical words that we’re finding in the media:
- An epidemic is an outbreak and spread of an infection (usually a communicable disease, though obesity is sometimes referred to as an ‘epidemic’) which is not usually active in a local population. In earlier reported stages of the Covid-19 outbreak it was considered to be an epidemic in Wuhan city, then in Hubei province and then in China. According to WHO in the case of ‘flu, an epidemic is declared if 0.4% of a population have the infection - in which case England and Wales has quite possibly not reached ‘epidemic’ levels of Coronavirus infection (0.4% of 60m people = 240,000 people; we have not had 240,000 people concurrently infected according to official figures).
- For ‘flu the UK defines an epidemic as occurring if the number of people consulting their GPs about it exceeds a certain level per 100,000 of the population. The four nations which make up the UK each have different thresholds:
| Country | GP consultations | |
|---|---|---|
| per 100,000 | ||
| Scotland | 419 | |
| N. Ireland | 142 | |
| England | 109 | |
| Wales | 75 |
- A pandemic is an epidemic that is no longer local - it’s gone worldwide. Covid-19 has been declared to be a pandemic by the WHO… and that’s the point. It’s a declaration by an official body that makes it a pandemic.
- Endemic is used to describe diseases that are always with us. The common cold is a great example. Nothing to see here - move along please. But just because a disease is endemic does not mean it is not deadly - every day some elderly or frail people die of ‘a cold’ (though there’s usually a co-morbidity). It’s not the cough that carried him off. It’s the coffin they carried him off in.
- Seasonal is often used to describe the behaviour of ‘flu. It starts spreading through the population and then it stops again after killing a few thousands of frail people and making many more feel very poorly. The speed with which the number of infections of seasonal ‘flu rise in England and Wales is astonishing - it’s almost as if it starts in multiple areas all at the same time. Where does it hide ‘out of season’?
There are technical definitions of these terms but not including just how big an epidemic has to be to be renamed a pandemic (great for headline writers but pretty much useless for most of us) or how often a bug has to come around for it to stop being an epidemic and be considered to be endemic or seasonal (I’m thinking of ‘flu here). Essentially they’re just degrees of the same thing. Diseases that spread and make people ill.
But what is ‘disease’ and a few other terms that are thrown around in the media?
- The term disease is often used to label a bug (eg to have Measles), but it really means ‘not well’; dis-eased=not well. The measles bug often causes disease but it is not a disease.
- Symptoms are indications that the individual notices in terms of changes to their health or ‘wellness’. Symptoms are often described as negative effects but it can be possible that some health issues result in the individual experiencing pleasant effects such as euphoria or unusual alertness.
- Signs are indications of a health issue that someone else can notice or measure. They are not directly subjective but may include reports of ‘symptoms’ from the individual.
A symptom of the disease Covid-19 may be losing the sense of taste which is not something that a doctor can directly observe. A sign that they have the bug may be that they report one of the known symptoms. A bad cough is both a symptom and a sign because both the individual and a doctor can observe it. A sign of Coronavirus infection might be a positive RT-PCR test - but we need to remain aware that a person with a positive test might be experiencing no symptoms and showing no other signs and not feeling diseased in any way.
Another area to look at is the use of the terms, ‘infection’ and ‘case’. It may seem to be nit-picking but there are crucial differences:
- Infection occurs when a bug (eg SARS-cov-2) gets into a host’s cells and they start to replicate it.
- A case requires a diagnosis.
A person can be infected but not showing any signs or experiencing symptoms. Without signs or symptoms they are unlikely to be diagnosed and so will never be counted as a case.
Another person may experience no symptoms but due to being a close contact of a previous case they may be asked to go for a ‘Covid’ test. If the test comes back positive they may be diagnosed as infected and so be counted as a case even though they are not diseased.
With most bugs there are usually far more infections than cases - that is to say, there are more people actually infected than formally diagnosed (consider for example, ‘flu). Unless there is a misdiagnosis every case has a corresponding infection; but not every infection results in a case.
The fine distinction between ‘infection’ and ‘case’ becomes important when we start to consider how dangerous a bug is. There are two main measures; Infection Fatality Rate (IFR) and Case Fatality Rate (CFR). Both measures refer to death, the ultimate end-point of disease, as a proportion of the other number. IFR is always lower than (or the same as) CFR because IFR is based on number of deaths divided by the number of infections. However, the CFR is easier to measure because it relies on actual diagnoses.
So, what is the CFR of Covid-19 compared with ‘flu?
- In England and Wales (according to PHE) there have been 41,902 deaths and 416,363 cases of Covid-19. Therefore the CFR is ~10% which would definitly put it in the ‘High Consequence’ category in my opinion.
- By early October World-o-meters shows ~36.5m cases and ~1m deaths due to Covid-19 to give a worldwide CFR of ~2.7%
- According to Wikipedia, seasonal ‘flu has a CFR of 0.002% and pandemic ‘flu a CFR of ~0.1%.
- PHE reports that 131,701 cases were identified from Pillar 1 and Pillar 2 tests (de-duplicated) in England and Wales during the month of September.
- At a CFR of 10% this would result in a further 13,170 deaths
- At a CFR of 2.7% this would result in a further 3,555 deaths
- At a CFR of 0.1% this would result in a further 132 deaths
- Mid-September to mid-October there were 1,644 deaths attributed to Covid-19 in England and Wales; this suggests a CFR of ~1.2%.
Mankind is resourceful and clever (and bloody arrogant). If we collectively get too upset about some bug then much effort is put into eradicating or at least controlling it. Smallpox used to be a killer but is now said to be gone. Polio was almost gone before suspicion of one group of mankind for another delayed (I hope only delayed) the end for it. A whole industry has grown up trying to nail down ‘flu each year and try to stop so many dying of it - but it’s a ‘cunning’ virus and keeps changing its coat (mutating) so our immune systems don’t recognise it each year. Many bacterial diseases were on the run but mankind’s mutual suspicion and arrogance has resulted in over-use and abuse of antibiotics which has given bugs respite and a chance to catch up in their evolutionary arms-race with mankind and TB still kills around 3,000 people per day. Again, there is much time and money spent to control HIV/AIDS but still it kills around 1,500 people worldwide each day.
It’s a very deadly plague…
No. No, it isn’t - at least not compared with many other diseases. There are some bugs which are more-or-less a death sentence if you catch them - the haemorrhagic fevers like Ebola spring to mind though they are mercifully rare. This Coronavirus bug is not in that league.
By early October about 36.5m people (0.45% of the world’s population of ~8bn people) worldwide have been confirmed as infected (see previous section) and over 1m people (0.013%) are said to have died. That is a lot of people killed but many/most were quite likely to soon die of something else. Many were already very sick with other diseases and got pushed over the edge by this infection - a concept called co-morbidity. Please don’t think I’m indifferent to people’s suffering; many people fear their own death and it’s a huge emotional shock when someone you love dies even if you were more or less expecting it. However, compared with many other bugs this Covid-19 virus is nowhere:
- Tuberculosis (TB) kills more than 1m people every year - that’s around 3,000 people every single day.
- Malaria kills about 750,000 people every year - that’s around 2,000 people every day.
- HIV/AIDS kills about 500,000 people every year - that’s around 1,500 people every day
To be fair, if you were to add those numbers up you’d be guilty of double counting which is another statistical sin. TB is a disease which commonly carries off HIV/AIDS sufferers - that’s a co-morbidity in those cases.
There was a sad report in the UK media about a young woman with no known co-morbidities who had died of Covid-19. It was sufficiently surprising that it made headline news even among the rest of the Covid-19 news. It also turned out not to be true - but they don’t hold the press while they check the facts.
Of course, Covid-19 could still have even more nasty surprises waiting for us. After all, this is a new bug. Perhaps some of those rate limiting mechanisms to the geometric progression thing won’t work quite as expected:
- Perhaps those who have apparently recovered will carry on infecting other people - that’s very unlikely but Ebola (for example) does something similar.
- Perhaps having caught it once will not confer any immunity - again, that’s unlikely but not impossible. If this were true it would also mean that we’re unlikely to be able to develop a working vaccine.
- Perhaps dying won’t stop you infecting others. Again, very unlikely, but Ebola (as an example of a ‘Contact’ infectious disease) can do this.
To try to put things into perspective: According to WHO figures about 57m people died in 2017 (around 156,000 people per day). That’s very roughly 1% of the world’s population - and that is normal. Some died in accidents, some in wars or by being murdered or executed, some from malnutrition and some from obesity (which at a stretch you could also call a type of malnutrition - mal=bad, nutrition=feeding: bad feeding). Many died from noncommunicable diseases such as heart disease, cancers, organ failure etc, some died as a result of poisoning or substance abuse or suicide, a few died from old age and many died from communicable diseases such as TB, HIV/AIDS, ‘flu etc. Respiratory tract infections (predominantly lower respiratory tract infections such as viral pneumonia) account for around a quarter of deaths worldwide.
Dying is natural. It does not signify failure. Everyone currently alive will do it eventually but nearly everyone tries to avoid dying sooner than they have to. The oldest among us exceed the age of 100 years but most die before that. It’s therefore no surprise that 1 in 100 (1%) of us die each year.
Much ridicule has been heaped on the PHE decision on 19 Mar 2020 to downgrade the Covid bug from being a ‘High Consequence Infectious Disease’ (HCID) just before the UK government imposed the tightest restrictions on people’s freedoms seen in peacetime in the past century. The bug was provisionally put on the list as ‘Wuhan novel coronavirus’ on 16 Jan 2020. PHE lists the HCIDs in two sections: ‘Contact’ and ‘Airborne’ which describes how these bugs are thought to spread among people. The current lists are:
Contact HCID
- Argentine haemorrhagic fever (Junin virus)
- Bolivian haemorrhagic fever (Machupo virus)
- Crimean Congo haemorrhagic fever (CCHF)
- Ebola virus disease() (EVD)
- Lassa fever
- Lujo virus disease
- Marburg virus disease (MVD)
- Severe fever with thrombocytopaenia syndrome (SFTS)
Airborne HCID
- Andes virus infection (hantavirus)
- Avian influenza A H7N9 and H5N1
- Avian influenza A H5N6 and H7N7
- Middle East respiratory syndrome (MERS)
- Monkeypox
- Nipah virus infection
- Pneumonic plague (Yersinia pestis)
- Severe acute respiratory syndrome (SARS)
There are a few things which struck me about these lists:
- The inclusion of Avian ‘flu H5N1 - which killed about 455 people worldwide (no, there’s no ‘thousand’ after that number) between 2003 and 2019.
- Many of the other bugs have horrendous reputations. Particularly Ebola, Marburg and Plague.
- SARS and MERS (both are coronaviruses) and the four ‘flus are in the ‘Airborne’ section - they are, after all, respiratory diseases. I don’t know which list the Covid bug was on but I would be surprised if it was not the ‘Airborne’ list.
- They are all viral diseases except for Pneumonic plague (Yersinia pestis) which is caused by a bacterium.
In removing the Covid bug from the HCID lists PHE added this explanatory note:
| Status of COVID-19 | |
|---|---|
| As of 19 March 2020, COVID-19 is no longer considered to be a high consequence infectious disease (HCID) in the UK. | |
| The 4 nations public health HCID group made an interim recommendation in January 2020 to classify COVID-19 as an HCID. This was based on consideration of the UK HCID criteria about the virus and the disease with information available during the early stages of the outbreak. Now that more is known about COVID-19, the public health bodies in the UK have reviewed the most up to date information about COVID-19 against the UK HCID criteria. They have determined that several features have now changed; in particular, more information is available about mortality rates (low overall), and there is now greater clinical awareness and a specific and sensitive laboratory test, the availability of which continues to increase. | |
| The Advisory Committee on Dangerous Pathogens (ACDP) is also of the opinion that COVID-19 should no longer be classified as an HCID. | |
| The need to have a national, coordinated response remains, but this is being met by the government’s COVID-19 response. | |
| Cases of COVID-19 are no longer managed by HCID treatment centres only. All healthcare workers managing possible and confirmed cases should follow the updated national infection and prevention (IPC) guidance for COVID-19, which supersedes all previous IPC guidance for COVID-19. This guidance includes instructions about different personal protective equipment (PPE) ensembles that are appropriate for different clinical scenarios |
Basically they’re saying that the HCID definition is not fit for this purpose - but did you spot this concerning the Covid bug? ‘…several features have now changed; in particular, more information is available about mortality rates (low overall)…’! Um, remind me again why we trashed so many people’s livlihoods?
Just one more thing on this: Did you also spot the bit about ‘a specific and sensitive laboratory test’? ‘Specific’ in this context refers to the test’s false positive rate (test says yes, but actually no bug present). ‘Sensitive’ in this context refers to the test’s false negative rate (test says no, but actually the bug is present). Although they’re giving no numbers they seem to be claiming that the test is accurate. See more on the accuracy of the tests below.
Counting the victims
At the time of writing, Italy (along with quite a few other countries) has been having a tough time of it. According to the excellent World-O-Meter, Italy currently (atToW) reports 101,739 infections (0.17% of their population). That number is made up of 71,547 who are currently infected with mild symptoms, 3,981 who are seriously ill, 14,620 who have recovered and 11,591 who have died. It’s notable that they do not report any positive tests with no symptoms. However you look at it, their death numbers are worryingly high… I mean no disrespect, but how reliable are the numbers?
On the face of it, counting bodies should be easy; surely things aren’t so bad that they’ve lost count? That isn’t the problem of course. The problem (if it exists) is in distinguishing between Covid-19 and other diseases. As far as a patient in intensive care is concerned they’re unlikely to care whether they’ve got pneumonia due to Covid-19 or influenza. Also, as far as a doctor is concerned the treatment of the patient is more or less identical*. Pretty much the only place it matters is in the paperwork - and that’s the problem. If a patient with cardiovascular disease suffers a heart attack and dies while suffering from Covid-19 then the paperwork might well say it’s a Covid-19 death and not due to a heart attack.
Imagine you’re a doctor with four patients who suffer from chronic obstructive pulmonary disease (COPD, ICD-10 J40-J44); they all have severe breathing difficulties.
Patient A’s breathing difficulties get a lot worse and then they die.
Patient B’s breathing difficulties get a lot worse and they’re tested for Covid-19 but the test comes back negative, then they die.
Patient C’s breathing difficulties get a lot worse and they’re tested for Covid-19 and the test comes back positive, then they die.
Patient D’s breathing difficulties get a lot worse and they’re known to have spent a lot of time recently with Patient C, then they die.
In each case what are you most likely to put as the cause of death?
Later you find out that Patient D had also spent a lot of time recently with Patient A and that a number of A’s family caught ‘flu shortly before he died. Does this affect your opinion?
The net effect is that you were ‘expecting’ to have to certify 4 COPD deaths sometime soon but you perhaps certified 2 Covid-19 deaths and ‘only’ 2 COPD deaths.
More likely, you certified 4 COPD deaths and mentioned Covid-19 as a contributory factor on two of them.
By the way, the last bit about Patient D above is there to highlight a peculiarity in the UK process for the registration of deaths. Once a death certificate is issued it cannot be changed. It can be added to but the original content may not be removed. The doctor certifying the cause of death needs to be cautious and not make assumptions.
Now imagine you are a doctor with a number of patients who suffer from ischaemic/coronary heart disease (CHD, ICD-10 I20-I25).
Patient E suffers what appears to be a heart attack and dies.
Patient F is tested for Covid-19 but the test comes back negative. They then suffer what appears to be a heart attack and die.
Patient G is tested for Covid-19 and the test comes back positive. They then suffer what appears to be a heart attack and die.
Patient H lives in the same care home as G. They suffer what appears to be a heart attack and die.
Again, you were more or less ‘expecting’ these patients to die relatively soon and you’ll probably certify them as CHD deaths, but you may add Covid-19 as a contributory factor to one or two certificates.
So why repeat what is essentially the same example? There is evidence that Covid-19 kills people with other ‘underlying health problems’ - not just respiratory problems. There’s also anecdotal evidence that it is killing more elderly people - but that should not surprise anyone. The older we get the more health problems we develop. It is rare for a person to continue in robust good health into old age and then just die - though most of us would wish that to be true.
There have been many reports in the media comparing Covid-19 with seasonal ‘flu and many claims and counterclaims that the comparison is right or wrong for various reasons. I would argue that it surely depends what features we are comparing. Clearly the economic impact of Covid-19 is far greater than with ‘flu (because of our knee-jerk lockdown reaction to it), but they’re both caused by viruses which spread in similar ways… but what about the death rate? One observation I would make is that nobody seems to be able to agree what the numbers for ‘flu (or Covid-19) actually are.
According to WHO (via Wikipedia), worldwide there are 3-5 million severe cases of ‘flu per year and up to 650,000 deaths (out of ~57 million deaths = 1.14%). However, in England and Wales ONS shows influenza (ICD-10 J09-J11) to be the underlying cause of just 576 deaths per year (576 deaths average 2014-2018, out of ~500,000 deaths per year = 0.12%). That seems to be out by an order of magnitude (10x too low).
One huge difference between ‘flu and Covid-19 is that many (probably most) cases of ‘flu are self-diagnosed whereas Covid-19 is (so far) mostly diagnosed via a laboratory RT-PCR test (Reverse Transcription - Polymerase Chain Reaction, similar technology to DNA profiling). In more normal times people tell their employer that they have caught the ‘flu and need to take time off work to recover - it makes sense to allow this as employers don’t need production being crippled by the spread of a disease like ‘flu around the workplace. In contrast consider our response to Covid-19 where we’ve preempted the spread of the disease by closing workplaces and crippling production.
In normal times if people are unwell they will tend not to go to the pub or visit friends or frail relatives partly to try to keep them safe and well and partly because they feel like death warmed over. Basically, we voluntarily do Social Distancing Lite. This demonstrably works - ‘flu comes in seasonal waves and more or less goes away again after spreading for a while and killing a ‘few’ frail people (usually 10,000-30,000 each year in England & Wales - see below).
Another big difference between ‘flu and Covid-19 is that there is usually a vaccine available against the prevalent strain of ‘flu. The vaccine is less effective in older people and in some years the vaccine is generally less effective than in others; not everyone accepts it even if it’s offered.
Public Health England (PHE) publish annual reports on the impact of ‘flu in England and Wales. The table below is extracted from Table 7 found on page 51 of the latest report and shows the number of deaths associated with ‘flu by age group in recent seasons.
| Season | All ages | 0-4 years | 5-14 years | 15-64 years | 65+ years |
|---|---|---|---|---|---|
| 2014/15 | 28,330 | 91 | 13 | 701 | 25,143 |
| 2015/16 | 11,875 | 84 | 11 | 1,259 | 9,459 |
| 2016/17 | 18,009 | 77 | 20 | 578 | 15,167 |
| 2017/18 | 26,408 | 6 | 2 | 1,462 | 22,237 |
So, according to PHE, in recent seasons deaths in England and Wales associated with ‘flu have been roughly 10-30,000 per season.
ONS publishes weekly, monthly and annual datasets of deaths in England and Wales. The Weekly datasets show total deaths registered and those which have been classified ‘J00-J99 diseases of the respiratory system’ and are also subdivided by age group of the deceased. These datasets are typically published 11 days after the end of the week being reported. The monthly datasets only examine where in England and Wales deaths were registered but offer no breakdown of the underlying causes. The annual datasets provide finer grained breakdown of cause of death and age group of the deceased but are summarised over the full year. They are usually published around 10 months after the end of the year being reported. The latest annual dataset covers the year 2018. The dataset for 2019 will be published in autumn 2020 and the dataset for 2020 will be published in autumn 2021. In addition, the data behind the published annual datasets is searchable using the nomis site.
PHE use the term ‘season’ to denote the period during which influenza-like illnesses (ILI) exceed a certain threshold level. It typically starts in the last quarter of a calendar year and ends some time in the second quarter of the following year. This variability in the meaning of the term makes comparing the number of deaths during PHE’s ‘flu season with the ONS’s annual or weekly statistics on deaths registered as due to respiratory or other diseases very difficult.
According to the ONS annual datasets the incidence of influenza as a registered cause of death is very low. ONS uses the International Statistical Classification of Diseases and Related Health Problems (ICD-10) to record causes of death. The list is very specific and is used by doctors to classify diseases, not just causes of death and as a result many codes simply do not appear in death statistics (for example, I would be surprised if anyone is registered as dying of H93.1 Tinnitus, though it can be a horrible condition). Influenza is classified under codes J09-J11.
| Cause of death | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|
| J09 Influenza due to certain identified influenza virus | 32 | 10 | 116 | 4 | 13 |
| J10 Influenza due to other identified influenza virus | 34 | 127 | 155 | 206 | 871 |
| J11 Influenza, virus not identified | 52 | 145 | 156 | 248 | 712 |
| J09-J11 Influenza | 118 | 282 | 427 | 458 | 1,596 |
So what’s going on? The answer is that unless the specific strain of virus has been identified, what gets put on a death certificate is a doctor’s opinion of what a person died of. A large majority of ‘flu deaths are not recorded on death certificates as ‘influenza’ deaths, but as ‘pneumonia, organism unspecified’. In other words, not the bug that the patient caught but the disease it caused that killed them. ONS only records what is registered on the death certificate and codes it accordingly. It appears doctors are rightly reluctant to register a death as influenza, a specific infection, when the death is really due to pneumonia, a disease arising from the infection. If we expand our search and look at codes J09-J18 (‘Influenza and pneumonia’) we find the numbers we were looking for:
| Cause of death | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|
| J09 Influenza due to certain identified influenza virus | 32 | 10 | 116 | 4 | 13 |
| J10 Influenza due to other identified influenza virus | 34 | 127 | 155 | 206 | 871 |
| J11 Influenza, virus not identified | 52 | 145 | 156 | 248 | 712 |
| J12 Viral pneumonia, not elsewhere classified | 37 | 47 | 57 | 46 | 66 |
| J13 Pneumonia due to Streptococcus pneumoniae | 83 | 87 | 121 | 104 | 122 |
| J14 Pneumonia due to Haemophilus influenzae | 6 | 10 | 3 | 2 | 8 |
| J15 Bacterial pneumonia, not elsewhere classified | 73 | 82 | 57 | 84 | 83 |
| J16 Pneumonia due to other infectious organisms, not elsewhere classified | 0 | 0 | 0 | 0 | 1 |
| J17 Pneumonia in diseases classified elsewhere | 0 | 0 | 0 | 2 | 0 |
| J18 Pneumonia, organism unspecified | 25,102 | 29,339 | 26,799 | 26,899 | 27,575 |
| J09-J11 Influenza | 118 | 282 | 427 | 458 | 1,596 |
| J09-J18 Influenza and pneumonia | 25,419 | 29.847 | 27,464 | 27,595 | 29,451 |
| J00-J99 Diseases of the respiratory system/* | 66,501 | 75,445 | 72,144 | 73,364 | 76,603 |
| A00-R99,U00-Y89 All causes, all ages | 500,314 | 528,507 | 523,857 | 532,130 | 540,265 |
/*I’ve reported ‘J00-J99 diseases of the respiratory system’ because it is presented as a subset of the weekly death statistics published by ONS (see below).
We must assume that what PHE refer to as ‘flu deaths are actually what ONS records as Pneumonia deaths where the cause is a bug but not actually specified. Another key difference is that PHE reports are based on ‘Seasons’ (eg Winter 2017-2018) and ONS records strictly on year (or week) of registration of the death - not necessarily on actual date of death.
ONS produce an annual figure for ‘Excess Winter Mortality’ (which corresponds quite closely to PHE’s seasonal figures) by comparing the average number of deaths registered in Aug-Nov and Apr-Jul of the following year with the number of registrations in Dec-Mar. This number is easy to calculate but can only be produced in the August following the winter period in question - once all the baseline data has been collected. As such it is no use for monitoring the progress of the current epidemic in England and Wales. Instead we can compare data gathered at around the same time in past years with data gathered this year almost as soon as the data becomes available. I have chosen to make many comparisons with the average weekly data of 2014-2018 (rather than ‘the past 5 years’) because the annual datasets only go up to the end of 2018 and I also wanted to compare the tail end of 2019 with preceding years average data.
WHO has defined new emergency ICD-10 codes for recording cases of Covid-19:
- An emergency ICD-10 code of ‘U07.1 COVID-19, virus identified’ is assigned to a disease diagnosis of COVID-19 confirmed by laboratory testing.
- An emergency ICD-10 code of ‘U07.2 COVID-19, virus not identified’ is assigned to a clinical or epidemiological diagnosis of COVID-19 where laboratory confirmation is inconclusive or not available.
The first code is only for when the laboratory RT-PCR test has been done, the second code is for if the test has not been done but in the doctor’s opinion the patient has (or had) Covid-19.
Although the U07 codes may be useful if they are used consistently no doubt many Covid-19 deaths among respiratory disease and other patients will continue to be coded as before. We will need to continue to be careful when counting victims to make sure we are including the correct data. The number least subject to opinion, and so most reliable, is the number of all-cause deaths.
ONS has been publishing its weekly datasets showing ‘Deaths registered weekly in England and Wales, provisional’ since at least 2010. These datasets show total (all cause) deaths and deaths where the ‘underlying cause’ is ‘J00-J99, diseases of the respiratory system’. It has started to include the new Covid-19 codes in its latest datasets where Covid-19 has been ‘mentioned’ on the death certificate but that introduces a potential inconsistency. They say: An ‘underlying cause of death’ refers to the main cause of death, whereas a cause being ‘mentioned on the death certificate’ means that it might be the main reason or a contributory reason to the cause of death. In other words the deaths recorded against U07.1 and U07.2 may be in addition to or may be part of the numbers recorded against J00-J99 ‘diseases of the respiratory system’ (or other unspecified underlying causes). In other, other words, these numbers may or may not be double counting - and we can’t know which. 10 years of valuable data made less meaningful by added vagueness. All we can do is compare the U07.1 and U07.2 numbers with the total (all causes) numbers.




One particularly interesting point: If we assume that the UK interventions of introducing ‘social distancing’ (16 Mar 2020) and school closures (20 Mar 2020) and full ‘lockdown’ (from 23 Mar 2020) actually had the desired effect of slowing down the spread of the virus then the peak number of infections must have occurred at around that time - let’s say around 20 Mar 2020 (week 12 of the year). The peak number of all-cause deaths were registered in weeks 16 and 17 of the year - 2 weeks centred around 17 Apr 2020. It typically takes 5 days to formally register a death so peak deaths must actually have occurred around 12 Apr 2020 (week 16) - about 23 days (~3 weeks) after peak infections. In other words it takes around 23 days (plus around 5 days if you only look at formally registered deaths) to see if a change in intervention results in a change in the number of deaths. The strict lockdown began to be eased on 17 May 2020 (week 20/21) - but ‘social distancing’ and school closures remained in force. Any increase in infections resulting from this change should have resulted in an increase in deaths starting around week 24 and registered around week 25. There is no such increase in ONS’ figures. From this I strongly suspect that ‘lockdown’ was not effective or necessary.
- If the peak of infections occurred before the interventions then the interventions were not the cause of the decline in infections - the interventions were not necessary (or effective).
- If the peak of infections occurred after the interventions then the infections must have continued increasing despite the interventions - in other words the interventions were not effective (or necessary).
- Easing the interventions did not result in an increase in the rate of deaths - in other words the interventions were not effective or necessary.
If we look at the chart of respiratory death registrations (deaths where the cause of death was coded in the ICD-10 J00-J99 range) we can see an unusual increase in weeks 13-17 of 2020 compared with previous years. I would suggest that these are misdiagnosed/miscoded Covid-19 related deaths; they should have been attributed to U07 rather than J00-J99. Similarly there is an unusual decrease in the respiratory death registrations from week 19 onwards. I would suggest that the decrease is due to deaths which would normally have been coded J00-J99 being coded as U07 instead. To avoid doubt, I’m suggesting the spike in death rates was actually worse than reported - and that misdiagnoses do appear on death certificates.
So is 2020 shaping up to be a bad year or not? Certainly something bad has happened from week 14 when 16,387 deaths are registered (it is worse than week 2 of 2015 when 16,237 deaths were registered). All cause deaths were up 60% while deaths due to diseases of the respiratory system were ‘only’ up 34% on the 2014-18 average for that week.

There are many possible interpretations of the numbers from week 14 but two opposite extremes are:
- All the deaths coded in the ICD-10 U07 category are actually ‘underlying causes’. In other words Covid-19 is the main cause of death in all these cases.
- All the deaths coded in the ICD-10 U07 category are actually ‘contributory factors’. In other words the main cause of death in these cases is something other than Covid-19.
If Covid-19 is effectively a respiratory disease then in each above case if we remove the respiratory deaths and Covid-19 as main cause from the total number of deaths we find the number due to other causes (ie not respiratory and not Covid). Which we can compare with the 2014-2018 average:
Extreme case 1:
Total - Covid - Respiratory = Other_deaths
16387 - 3475 - 2106 = 10806
Extreme case 2:
Total - Respiratory = Other_deaths
16387 - 2106 = 14281
2014-2018 average:
Total - Respiratory = Other_deaths
10268 - 1573 = 8695
From the above we see that in week 14 of 2020 we have registered between 2,111 and 5,586 more deaths due to ‘other causes’ than the 2014-2018 average.
The truth will be somewhere between the two extremes. It may be that the infection is killing off (say) CVD (ICD-10 I00-I99) sufferers but that the deaths are still coded as CVD… but it is also possible that people are dying from other preventable (or at least delay-able) causes while the country focuses on Covid-19. Unfortunately the weekly datasets do not go into enough details to tell.
Just one more point on this: in the UK, ‘lockdown’ effectively started half way through week 13. The spike in death registrations became significant in week 14. Death registrations are normally required within 5 days of death. Are these extra ‘unexplained’ deaths actually caused by the lockdown?
Just by the way, and by comparison, dying of ‘old-age’ is considerably less usual than dying of respiratory diseases and runs at around one tenth of the J00-J99 deaths each year or 1.5% of all deaths.
| Cause of death | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|
| R54 Senility | 7,700 | 8,177 | 7,754 | 7,661 | 8,038 |
The ONS annual datasets offer a finer breakdown of causes of death than the weekly ones… but they lose the detail needed to identify short-term trends (such as the weekly progress of an epidemic). From the annual datasets (latest figures now cover 2019), during 2013-19 around 5.7% of deaths in England and Wales were attributed to ‘flu and pneumonia (J09-J18, mostly attributed to ‘flu by PHE). Each year’s data are usually published in November of the following year. It will be interesting to see the corresponding stats for 2020 when they’re published in November 2021. On the principle that someone can’t die of both ‘flu and Covid-19 I expect we’ll see an overall drop in one number and an increase elsewhere. I hope I’ll be around to say ‘I told you so’. Until then we will have to rely on the provisional (ie subject to revision if necessary) weekly stats published by ONS usually published about 11 days after the close of each weekly period - even though they warn us within those datasets that they may commit the statistical sin of double counting.


All the discussion about death rates and causes tends to obscure the fact that for most people the most likely outcome of reaching a certain age is actually surviving to get a bit older. In other words: What are your chances of life? Here’s a chart of most likely outcomes depending on age group drawn from the ONS annual death registrations dataset and mid-year population datasets. To try to explain it better: If you’re male and you’ve survived to reach the age of 90 then you have a 78% chance of making it to 91; this year your chance of dying of cancer, 3.6%; ‘flu/pneumonia, 2.4%; mental health problems (eg dementia), 3.6%; old age, 1.1% and so on add up to your 22% risk of death. The younger (and more healthy) you are, the higher your chance of surviving to see another birthday. Not too surprising if you pause to think about it. Note that the overall risk of dying does not even amount to 1% until agegroup 65-69 for males or 70-74 for females.


So what would those charts look like in 2020?


Now, for which outcome are you going to spend the most effort preparing? Choose life. Life is for living.
Anecdotal news is emerging that lends support to the idea that deaths from various different conditions are being attributed to Covid-19. This report published in the New York Times (usually paywalled) suggests that the pandemic has coincided with a dramatic fall in the number of cardiovascular disease (CVD) cases being seen at hospitals. The article explores a number of possible causes for this observation, including that people are just toughing it out and not seeking help when they apparently should - but if that were the case I’d expect to see an increase in CVD deaths, unless a significant proportion of medical interventions on CVD are actually pointless. It is not a rigorous analysis - for that we will have to wait for the numbers to be collected and the dust to settle.
From the above section it should be clear that ‘counting deaths from Covid-19’ is not as simple a task as it at first appears it should be.
Is COVID-19 targeting…
Is COVID-19 targeting the elderly? Well… no, not really. Yes, more of the ‘elderly’ are dying of this bug than any other age group, but not disproportionately more so. For quite some time ONS weekly datasets have included a breakdown of deaths by age group. The most recent datasets in 2020 have finer divisions of age ranges but they can easily be aggregated to compare with the agegroups used in previous years. These datasets show that between 2010 and 2019 around 40% of the deaths registered each week are of people aged 85+ and about 28% are people between 75 and 84 years (ie 68% of deaths are over 75s).

This ratio does not change significantly over the years and only slightly by season of the year and has not significantly changed in 2020 when compared with other years.
| Age group | Percentage of |
|---|---|
| deaths/week | |
| below 1 year | 0.4% |
| 1-14 years | 0.1% |
| 15-44 years | 2.4% |
| 45-64 years | 11.5% |
| 65-74 years | 16.1% |
| 75-84 years | 28.6% |
| 85+ years | 40.8% |
Remember that these are percentages of all those that die in a week - and not that ‘40% of people aged 85+ die’ in any particular time period. Of course, 100% of people aged 85+ die… eventually.
Is COVID-19 targeting males more than females? Again, not really. Essentially the same proportion of males:females are dying during the epidemic as have done during normal times since Jan 2010.

The proportions of male:female deaths and age of death has not changed significantly for any age group during the epidemic. The inequalities in death rates between males and females in each age group has remained the same but the overall numbers of deaths has increased.

This bug doesn’t ‘target’ the elderly or men in particular - it targets those susceptible to death. If you are more unhealthy than other people your age and sex, you are at greater risk of dying than they are - but then you knew that already, didn’t you?
The striking historical imbalance in the ratio of males and females dying in each age group deserves some exploration. Marginally more males than females are born so the starting ratio among early years is slightly more males than females. In each agegroup except the 85+ group, more males than females die (in other words males die earlier than females). This has the rather obvious effect of resulting in the female:male ratio gradually increasing as the population ages until in the 85+ agegroup there are nearly twice as many females remaining as males - and given that all of us will die eventually, that sets the final ratio of female:male deaths in this agegroup.

Click here for an animated 3D chart of week by week deaths by age group for Males and Females in England and Wales from Jan 2014 to date.
Is COVID-19 targeting BAME (Black, Asian, minority ethnic) people? Well, so the media reports say, but the same media also imply that it affects the elderly and men disproportionately (but it doesn’t). This is a sensitive subject (I mean the subject of disproportionately bad outcomes for BAME people generally) and much research has started into why this might be in the case with Covid-19. We’ve seen above that there are changes to the male:female ratio of the population depending on age. Is there any similar change in the BAME:non-BAME ratio depending on age which might partially account for the difference in death rates? Is the difference related to different population age distribution or immigration/emigration dates or social or economic deprivation or behaviours or genetics? It is known that Asian people are more susceptible to type II diabetes than ‘white’ people and that diabetes is a co-mobidity for Covid-19; also, sickle cell disease is more common in people of African descent. Are these and similar conditions enough to explain the difference in death rates during the epidemic? Even if they are, it just moves the problem to explaining the disproportionate prevalence of these conditions in different ethnic groups. If the differences are caused by genetics then there’s not a lot we can do about it - but such a discovery will be useful science and may help us identify and protect the vulnerable.
Across the UK BAME people make up different proportions of the population. The following chart shows the ethnic make up of the various countries of the UK, the UK as a whole (and then England and Wales together) and is drawn from a 2016 report by ONS based on the 2011 census.

According to the data, non-‘white’ people make up 14.87% of the England and Wales population. The question is do BAME people make up significantly more (or fewer) than 14.87% of Covid-19 victims - and if so, why? ONS do not include any indication of ethnicity in their death registration datasets so we cannot explore the facts based on that data - and I don’t have the skills or knowledge to speculate further.
Is COVID-19 targeting care home residents? Yes, sort of. Possibly as a reaction to media reports of disproportionate numbers of deaths in care homes, starting in week 13 of 2020 (the week lockdown began), ONS began to include information on the type of place that people in England and Wales die (including retrospective information from the beginning of 2020). From this we can extract the data for the following chart:

The chart shows that the proportion of deaths that occurred in the various places didn’t vary much between the average of Weeks 1-10 and Weeks 11, 12 and 13. As the overall number of deaths also didn’t rise significantly above the long term average during those weeks we can safely call this period ‘normal’. During this normal period about 46% of deaths occurred in hospital, 23% in care homes and 24% at home - the other categories being hospices, other communal premises (prisons, barracks, hotels, student halls of residence etc) and ‘elsewhere’ (roads, workplaces, holiday accomodation etc).
The fact that, in normal times, 23% of deaths occur in care homes should not come as a huge surprise. A care home is a place where people go to live when they can’t care for themselves - they need care from others. In the majority of cases this will be elderly people who used to live independently but now find it too difficult to cope in their old homes. The majority of care home residents are elderly and frail - almost by definition of what a care home is for. In normal times, and during the Covid-19 epidemic, the majority of deaths occur among the elderly (68% of deaths each week are people over 75). So a large proportion of deaths are likely to be among care home residents.
Prior to the epidemic about 250,000 people lived in care homes in the UK and about 2,500 (1%) died each week and were replaced by new residents who may have been waiting for a place to become available. During the eight week period covering the peak of registered deaths in the UK about 2% of care home residents died each week.
What is particularly disturbing is the way that the chart shows that the percentage of the deaths during the peak of the epidemic skewed away from hospitals towards care homes. The accusation in the media is that in the rush to clear the hospitals to prepare for an expected influx of Covid-19 patients, the NHS unreasonably discharged infectious elderly patients to go back to their homes to recover (or if not, to die) - even if those patients lived in care homes where many other vulnerable people lived. I would suggest that the cause of this was not malice but administrators blindly following a policy set by senior NHS managers (to clear the hospitals) without consideration of the individual circumstances of the patients (living in care homes). When/if there is a public enquiry into this aspect of the epidemic in the UK I believe this will be one of the findings: top-heavy, not medically informed or educated bureaucracy in the NHS; another finding will be a disconnect between the policies of the NHS (short-term treatment) and social care (long-term support).
The ‘new normal’ since the peak of Covid-19 deaths seems to have settled with 39% of deaths occurring in hospital, with 20% in care homes and 33% of deaths each week occurring in private homes. Rather than redress the balance it now seems more people are expected to die at home than before the peak of the epidemic.
How can we protect the residents of care homes without turning them into prisoners? The answer is of course isolation hospitals or ‘sick bays’ where residents who become unwell are treated or nursed until they either recover or die - not leaving them in close contact with the other residents. I know it’s a radical thought but how about we use hospitals to treat sick people and leave care homes to be… homes. It seems to me that this would have been a sensible use of the ‘Nightingale hospitals’ which were commissioned at the height of the panic - and then barely used.
Is COVID-19 targeting dementia sufferers? There has been a huge increase in deaths among dementia sufferers but pretty much all people with significant dementia live in care homes. I am not convinced that the Covid bug is to blame beyond the care home effect. I think many of these additional deaths have been precipitated by the lockdown and prohibition of care home visits.
I heard a recruitment advertisement on radio in March (I think), something along the lines of: ‘We’re the NHS. We’re 1 million people and growing…’. I don’t know whether that number was referring to NHS England or the NHSs of the whole of the UK but let’s assume it was the whole of the UK. Children and retired are presumably not included and about 25% of ‘working age’ people do not work, so 1 in 33 (rough estimates: UK population 67m, 66% ‘working age’, 75% actually working = 33m workers) of all working people in the UK are ‘in the NHS’… and they’re still growing. Does this seem reasonable to you? 3% of all workers (public and private sector) in the UK are NHS? That said, 19% of government public spending (central and local government) is on healthcare. Not enough? Just right? Too much?
A coat of motley
A jester (or ‘fool’) would wear clothes made up of many different colours and pieces in order to poke fun at fashions - or more at the people wearing them. They were said to be wearing ‘motley’. If the current fashion was to wear a pleated ruff around the neck then a jester might wear one much bigger or much smaller or more tightly pleated or floppier or more brightly coloured than anyone else; or for kilts, much shorter or longer or wider or multicoloured than usual; or for codpieces… well, you get the idea. You couldn’t accuse them of not joining in with the fashions of the day - but there was always something wrong with how they did it - for comic effect.
An influenza (or ‘flu) virus (there are many, just like coronaviruses or rhinoviruses) has many different ‘coats’. As it circulates among and infects people their immune systems begin to recognise the coat the currently circulating virus is wearing and prevent it from attaching to more cells in the body and doing any more damage. This is why it’s rare (but not impossible) to catch the ‘flu twice in a season - if recently infected, a person’s immune system recognises the bug from it’s coat and if a new infection starts already knows how to deal with it. By taking samples from infected people and analysing them scientists have learned to label these virus coats as ‘HxNy’ types (where x and y are numbers). Examples include:
- the swine flu pandemic which caused much alarm in 2009/10 (150-575 thousand deaths) was an H1N1 ‘flu virus just like the extremely deadly Spanish flu of 1918 (17-100 million deaths).
- the Hong-Kong flu of 1967-8 (~1 million deaths, 30,000 in England and Wales) which was an H3N2 ‘flu virus.
- the Asian flu of 1957 (1-4 million deaths) which was an H2N2 ‘flu virus.
- the avian flu scare of 2004-2007 involved a pandemic among wild birds and poultry with a few infections and deaths (~455) among people. The fear was that the bug might mutate to infect and kill large numbers of people.
Most ‘flu does not provoke a long-lasting immune response unlike some bugs. After a few years a person’s immune system might ‘forget’ how to deal with (say) H1N1 ‘flu and so be slow to respond if they get infected by it again.
This variability in ‘flu is what makes it able to come back year after year and infect people and be ‘successful’. If it always looked the same and tried to come back year after year eventually it would become like chickenpox and mostly infect only small children whose immune systems have never encountered it before.
‘Flu is a deadly disease, it is said to kill around 1,000 people per day worldwide (though that’s considerably fewer than TB). This has upset mankind and we have collectively started to do something about it. In temperate countries ‘flu mostly spreads during winter months as it is most easily transmitted as people gather together in warm houses and offices to stay in from the cold outside. Of course, it also spreads in tropical countries as people gather in air-conditioned spaces to stay in from the heat outside - but that isn’t seasonal so we don’t spot its seasonal nature in tropical countries. The key point is that it spreads when people gather together.
The fact that people rarely caught the ‘flu twice in a season seemed to offer some hope for developing a vaccine, but early attempts were rather hit and miss. Sometimes a new vaccine worked and sometimes it didn’t. A vaccine might start off quite effective and then the same preparation would fail miserably in a trial a few months later. Then a new vaccine would be developed and tested and would work for a few months before it too failed. It became obvious that the ‘flu bug was different with each wave of infection which seemed to mean that to be effective a vaccine would have to be developed and distributed and administered within weeks of the start of each ‘season’ in order to disrupt the ‘geometric progression’ phase of infection each year - an impossible task.
However, the seasonal nature of ‘flu does mean that industry can try to predict what coat the next infection will be wearing - by looking at what it’s wearing in the current ‘flu season in the opposite hemisphere - and so have more time to prepare, distribute and administer vaccines to train people’s immune systems before the next wave of infection arrives. Often industry gets it right and the vaccine prevents the vulnerable from dying of ‘flu that season; but sometimes the prediction is wrong and the vaccine is ineffective and then you get many more deaths among the vulnerable.
The need for a new vaccine each season is a huge opportunity for the businesses creating them. It’s regular work in that it needs re-doing each year. Everything from researching which strains are currently circulating and predicting which will be circulating, to producing the vast numbers of ampoules of vaccine and distributing them to the customers is a well practised process which is carried out efficiently year after year.
I’ve described the ‘flu vaccinations above as being a function of industry: In the UK, the NHS buys vaccines from pharmaceutical companies and pays General Practitioners and others to administer them and keep records. In other parts of the world your healthcare insurer may do this instead or you may have to pay a clinic directly. The pharmaceutical companies make money out of this which helps to keep them in business so that (among other minor things like making a profit) they can spend resources creating next season’s vaccines.
Resistance is futile!
Not so. At least, not if you’re a bug.
If someone has a bacterial infection and their natural immune system is failing to fight it off then doctors can give that person antibiotics to try to kill the bugs. Antibiotics typically work in a reverse of a geometric progression as described above and are often initially given as a 7 day course. The first day the antibiotic kills (say) half the bugs in the patient’s system and stops the rest replicating for a while. Each subsequent day it kills off half of the remaining bugs and stops the rest replicating for a while longer. After 7 days of taking antibiotics there are less than 1% of the original number of bugs remaining and the patient’s immune system should be able to finish the job of killing them off… But what happens if someone has an ineffective immune system? They have to keep taking the antibiotics for longer until all the bugs in their system are dead.
Something that often happens is that patients start to feel better as the number of bugs in their system reduces. So they think they’re cured and stop taking the antibiotics after a couple of days. The remaining bugs restart replicating and the disease begins to come back - but this time the new generation of bugs are replicated from those bugs which survived the initial doses of antibiotics; they are more resistant to the drugs and can take longer to clear. When this effect continues it can even become impossible to cure the disease with antibiotics. Even worse than this the patient can pass on the resistant bugs to the next victim who now catches a drug-resistant disease.
Some strains of tuberculosis have achieved this resistant status - which helps explain the high death rate mentioned above. If they are resistant to two of the usual antibiotics they are known as Multi Drug Resistant TB (MDR-TB). If they are resistant to many of the usual antibiotics then they are known as Extensively Drug Resistant TB (XDR-TB). To treat MDR-TB patients require at least 6 months and sometimes as much as 2 years of antibiotic treatment which can be damned expensive for the individual in countries without an NHS.
The drugs don’t work
So why can’t we just take a course of drugs to beat the bug?
The problem is that the Covid-19 bug is a virus and not a bacterium or parasite and that pretty much all virus diseases are not curable by drugs. There’s no such thing as a general antiviral drug. The best that can usually be done is to help the infected person survive or feel better while their immune system works out how to stop the virus replicating. That’s really bad news for people with poor immune systems like the elderly or cancer or organ transplant patients.
A complication can arise if a person’s immune system is too aggressive. The immune system starts by killing off infected cells as it’s supposed to, but it then goes wild and starts killing off uninfected cells - cells which are needed by the body and without which the host cannot survive. That might be listed as a death caused by the bug - but it’s really an autoimmune disease death. One drug that has shown promise in this area is Dexamethasone; a relatively inexpensive corticosteroid which promotes healing of the damage done by Covid-19 by regulating immune responses.
The reason that most drugs don’t work on viral diseases becomes clearer when you think of the differences between these three types of infection:
- Multi-cellular parasites typically live in voids within the host body. For example, worms living in the guts and feeding on nutrients there. A course of worming agent through the intestines can usually clear them out. They’re often visible to the naked eye (several millimetres, 100-1,000 times bigger than bacteria)
- Single cell organisms which live between the cells of the host body. For example bacteria or yeasts that make room for themselves by releasing toxins to kill off adjacent body cells and feed off the ‘soup’ released from the dead cells. A course of appropriate antibiotics or antifungals carried around the body fluids will eventually reach most such bugs and should kill them off provided they have not developed resistance as described above. Bacteria are typically 10-100 times bigger than viruses (eg Cholera bacterium is 0.3 x 1.3 micrometres, 0.0003 x 0.0013 millimetres, or about 2,500,000 could be packed onto a square millimetre)
- Viruses are not what most people would consider to be living things. They have no cell wall and no mechanisms to take up nutrients (feed) or replicate on their own. To replicate they have to attach to the outer wall of a host’s cells and be actively drawn in by the cell (I’m sorry to admit I think of it like vampires being unable to cross the threshold without being invited in - and which is humourously consistent with the concept of viruses not quite being living things). Once inside the cell they hijack the internal machinery to make many additional copies of themselves and often in the process kill the cell. Basically the only way to get at them with a drug is either to prevent the virus attaching to the cell in the first place or to identify and kill all the infected cells before they can make more copies - which is very bad news if a very large number of the hosts cells have been infected. Viruses are typically 100nm in size (0.0001 millimetres, or around 100,000,000 could be packed onto a square millimetre). A potentially helpful comparison: Much study has gone into how bad diesel fumes are for city-dwellers and how difficult it is to keep the smoke out of people’s lungs; very fine smoke particles are around 1,000 times bigger than viruses.
One approach that can work in preventing virus diseases is vaccination. Vaccination is essentially teaching the body’s immune system to recognise and remove infected cells early and so prevent the replication of the virus. Or to generate sacrificial cells which the virus will attach to in preference to ordinary cells and which will take the virus particles out of circulation. Vaccines are usually specific to the strain of virus being targeted, so for example a vaccine against H1N1 ‘flu will not teach the immune system about H5N1 ‘flu and won’t stimulate immunity against it. Unfortunately, creating, testing, manufacturing, distributing and administering a vaccine for millions of people takes a lot of time and the Covid-19 bug is new to science. Apparently some groups have been experimenting already and have started Phase I clinical trials on healthy volunteers with a potential candidate but a vaccine for general use may still take 18 months or more to become available - if it doesn’t fail at Phase I or any of the other phases along the way. Releasing a vaccine and treating millions (or perhaps even billions) of people before it has been properly safety tested could be a nightmare - the ‘cure’ could be far worse than the disease.
Nobody knows if a vaccine to protect against the Covid-19 bug is possible. Mankind has never produced a vaccine against the other coronaviruses that afflict us (there’s no vaccine for the common cold, for example) but that may be just because the other coronaviruses didn’t annoy us enough to make the effort worthwhile. If it is possible to create a vaccine it may be too late to be much use - no lab bothered to follow through to create a vaccine against SARS or MERS because those pandemics fizzled out.
Even if it is possible to create a vaccine within the next year that does not mean that everyone will get it. The panic in developed parts of the world means they will pay pretty much anything to get it and will buy up all the supplies they can until enough people are vaccinated. Unless philanthropic groups fund it (like they do with polio vaccination) the vaccine will barely feature in the developing world.
Up until 2005 the UK used to routinely vaccinate young teenagers against tuberculosis (TB, a bacterial disease). The vaccine was referred to as the ‘BCG shot’ (BCG: Bacillus Calmette–Guérin vaccine). Children would be tested with a very small scratch test and if they already had immunity they would react with itching and/or swelling within a few days. If they did not react they would then be given the main injection. This blanket vaccination was replaced with a more targeted approach when TB became less common in the UK. The BCG shot has been available for decades… so why do 3,000 people per day across the world die of TB? The answer is that in less developed parts of the world families cannot afford to vaccinate their children. In the UK we pay for this sort of thing through our taxes funding the NHS, in countries without an NHS people have to pay their insurers or pay the clinic directly or rely on charity.
Vaccination and inoculation
Edward Jenner was an 18th/19th century physician who is widely recognised as a pioneer in vaccination. The term ‘vaccination’ refers back to the idea of inoculating subjects with cowpox (vaccinus=of or from cattle) in order to provide immunity to the much more dangerous smallpox. He was certainly not the first to do this but he is recognised as the first to test its effectiveness.
The practice of inoculating healthy young people with pus or scabs from recovering smallpox victims was not new (it had been going on for centuries) and Edward Jenner was inoculated in this way when he was young. The resulting infection and disease is said to have affected his health in later life.
In the late 18th century he conducted an experiment on the eight year old son of his gardener. He inoculated the boy with pus from blisters on the hands of a dairy worker who was recovering from cowpox (a zoonosis caught from infected cattle). After the child recovered from the resulting cowpox infection, Jenner inoculated him with material taken from a smallpox sufferer. The child did not develop a smallpox infection. Despite a repeat attempt to inoculate the child with smallpox he remained disease free.
The above experiment is not quite as unethical as it at first appears. In the normal course of events Jenner would have been paid to inoculate the child with smallpox and then manage the course of the infection and disease until he recovered - the intention being that a child would be more likely to survive a managed bout of the disease (and so become immune to future infections) than an unmanaged infection. By inoculating with cowpox he was introducing a much less dangerous infection. However, Jenner’s repeated attempts to inoculate with smallpox after the child recovered from cowpox would have most modern medical ethics boards in a rage.
Modern vaccines are not nearly as dangerous as transferring infected material from one patient to another but they still aim to provoke the immune system of the recipient into reacting to the vaccine as it would or might eventually learn to do with a real infection. I sincerely hope nobody is trying an 18th century inoculation approach to developing a vaccine for the Covid-19 bug. No, no. You first. I’ll take mine after you. No, I insist…
After writing the above paragraph I found this article on the BBC News website. It seems 18th century medicine is alive and kicking!
On 8 Nov 2020 the UK Government issued this announcement: Social media giants agree package of measures with UK Government to tackle vaccine disinformation. A week later the UK’s main opposition party suggested that Emergency laws to “stamp out dangerous” anti-vaccine content online should be introduced. Presumably broadcast and subscription media had already submitted to the editorial control of the Ministry of Truth.
In the year 2000 the UK introduced seasonal ‘flu vaccinations for the vulnerable and over-65’s. As can be seen from the first chart in this post it appears that this significantly reduced the number of excess Winter deaths in England and Wales in subsequent years.


However, there was and is no corresponding effect on the all-cause annual death rates or age of death. It would appear that deploying the vaccine smoothed out the seasonal ‘bumps’ in death rates but didn’t result in people living much, if at all, longer. It reinforces the view that most of the victims of ‘flu are those who are frail and ready to die from the next bug that comes around.
The steady improvement in death rates (most probably due to interventions like improved neonatal care and campaigns against smoking) for each agegroup continued on as they had done for the previous 50 years without any significant change. It raises the question if the cost of the ‘flu vaccination program (around £115m/yr in 2010) could be better spent on other health interventions.
Again, don’t get me wrong: I’ve had ‘flu a couple of times in my life and it’s horrible. I certainly don’t want to catch it again. If I do catch it again I don’t want to pass it on to anyone else. Also, it may be that the cost to the NHS of the ‘flu program is justified by less lost productivity in the workplace - but if so, only giving it free to the over 65’s seems a strange tactic.
Drastic action… We mustn’t panic!!
- It’s not as deadly as TB - or even some ‘flus.
- The majority of deaths are among the elderly and frail (like with ‘flu).
- It will not continue to spread at the same rate it has been. Indeed, it may already be everywhere.
- Maybe we can slow down its spread (I’m not convinced) but we can’t actually stop it (without a vaccine).
- We must make sure the steps we take to control Covid-19 are not worse than the disease itself.
So if it’s not so very deadly, and most of those that it is killing were relatively close to death already and it can’t continue to spread at the rate that it started but can’t really be stopped either, why have the governments of the world taken such drastic action? The clue is above: some people ‘require treatment in hospital to recover’. The government policy was not intended to stop anyone catching it - that’s impossible now and in any event is pretty much up to the individual to achieve. The policy is to stop loads of people catching it all at the same time and overwhelming the hospitals.
Death is one of the least likely outcomes of a Covid-19 infection. Anecdotal reports suggest that most will feel a bit unwell and then get over it or possibly not even notice - but some will be very unwell and will need hospital or even intensive care to get over it. If all the ICU beds are occupied or there are insufficient ICU staff then some people will die for lack of treatment; this is what the government policy is seeking to avoid. Once again let’s use some simplified numbers to try to get a handle on this.
Let’s imagine a FICTIONAL bug which WILL infect everyone in our FICTIONAL world. About 90% of the infected WILL get better 1 week after catching it. Of the other 10%, half WILL die no matter what we do and half WILL get better but only if they get hospital treatment - but we can’t tell which half. Trouble is we only have hospital space for 1% of the population.
At first glance this is truly dreadful: 10% of our population must go into hospital to have any chance of survival but we only have space for 1%. So 9% of our population is doomed and we have the horrible task of deciding which 9% of the population we’re going to allow the bug to kill. Of the 1% we do put in hospital half will die anyway so it looks like we’re actually going to lose 9.5% of our population.
But maybe it is possible to limit our loses to 5% of the population - and therefore literally save 4.5% of our population from this bug. Tell everyone to spread out and stop making it easy for the bug to jump person-to-person. This slows the bug down enough so that only 10% of the population have it at any one time. Of that 10%, one tenth (1% of the population) need to go into hospital to stand a chance of survival. Fortunately we have hospital capacity for 1% of the population so nobody gets left out. Of that 1% half survive and half die = 0.5%. 1 week later we let another 10% of the population catch it and expect that a further 0.5% of the population will die. Repeat this process a further eight times and then we can remove the restrictions on people because everyone has caught it and everyone who could be saved has been saved.
Did I mention that this bit is about a FICTIONAL bug in a FICTIONAL world?
The example above is obviously fictional because we knew exactly what numbers were going to catch it (everyone, 100%), how many of those were unquestionably going to die (5%), how quickly people would either get better or die (1 week) and how much hospital capacity we had (1%). The only thing we could control was the speed of spread and we used that to prevent any excess deaths. We also had a very obedient and trusting population, another fiction.
Of course, closer to reality, because it’s so new we don’t have a really good estimate of how many are likely to catch the Covid-19 bug or how soon or for how long or how many will need hospital treatment or how many will die - and we don’t have very obedient or trusting populations either. So all our governments can really do is listen to the scientists they trust most and try to balance the anticipated harm of any intervention against its benefit.
One interesting feature of the scientific advisory group that the UK government has convened is that it is made up of experts in a number of different fields:
- New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG)
- Scientific Pandemic Influenza Group on Modelling (SPI-M) (Department for Health and Social Care)
- Independent Scientific Pandemic Influenza Group on Behaviours (SPI-B)
From the constitution of the group it certainly appears that the experts think Covid-19 is a respiratory disease with some similarities to ‘flu. It is also notable that there is no representation of economists in the group - but I guess that’s because if they had two economists they’d end up with three different opinions.
As individuals we can try to buck the trend and try not to catch the bug at all or we might reckon we know better and ignore our governments’ advice. Some people go to extreme lengths to avoid catching diseases and with very deadly diseases such as Ebola that makes a hell of a lot of sense to me. Equally, some people are reckless and continue to engage in risky behaviour (like smoking) despite their government’s advice. But Covid-19 is nothing like as deadly as Ebola or as easy to avoid as smoking. For most people it will just be a rather bad cold - but just in case you do catch it, try not to pass it on.
Tests, tests and more tests
In mid-March the WHO issued a statement: Our key message is test, test, test. It sounds like a ‘no-brainer’ - of course we should test so we can find out everything about this bug. The trouble with no-brainers is that if you don’t think about them you can draw the wrong conclusions.
There are two main types of test for viruses like this bug:
- RT-PCR type tests which are designed to find signature fragments of the virus and multiply them up (replicate them) until you have enough material to confirm the presence of the bug
- Antibody tests which are designed to detect whether a person has developed antibodies to this virus - and so, by inference whether the person has had the bug in the past.
PCR tests are useful in forensic examination of crime scenes in that the tiniest trace of a suspect’s DNA can be built up to confirm the presence (or not) of the suspect at a particular scene. The test returns a yes/no (actually, detected/not detected) result with almost no indication of the amount of DNA in the sample. It’s either there or it isn’t. Unfortunately, these tests are prone to errors caused by contamination - for example if two pieces of evidence obtained from separate locations are allowed to come into contact with each other then a PCR test might return ‘detected’ for both even if only one was actually handled by the suspect. The handling of evidence for DNA testing is very carefully controlled to prevent this sort thing happening - after all, the freedom of a person might be at stake. When DNA forensic evidence is presented in a court of law it is often used to prove that a particular suspect was at a crime scene sometime in the relatively recent past with an expert giving guidance on length of time the DNA would remain detectable on the sample and how unlikely a false positive result might be. It is not assumed to prove that the suspect is still at the scene; they’re usually in the dock.
When developing an RT-PCR test for a new virus researchers need to identify ‘signature’ fragments which are unique to the bug in question (for example, in the case of the Covid-19 bug they musn’t be present in other coronaviruses), the signature fragments must be unlikely to change as the virus mutates/evolves over time and also not so fragile that they decompose during the time between the sample being taken and the test being run. In addition they should not be fragments which are produced as the body’s immune system breaks up viable virus - the test needs to detect viable virus, not destroyed virus. One more thing: it needs to be fast - getting the result days later is no good.
| A PHE spokesman has been quoted as saying | |
|---|---|
| “It is important to note that detecting viral material by PCR does not indicate that the virus is fully intact and infectious, i.e. able to cause infection in other people. The isolation of infectious virus from positive individuals requires virus culture methods. These methods can only be conducted in laboratories with specialist containment facilities and are time consuming and complex.” |
Unfortunately, the initial RT-PCR tests that were developed for the Covid-19 bug have a poor reputation for false negatives (the patient apparently does have the bug but the test says not). Obviously, repeated testing could identify these failures - or they might actually show that these people had some other bug and really didn’t have the bug at the time of the test. But how to find out which? More research is required.
In addition it has been reported that most people who test positive have no symptoms on the day of the test. However, 78% reported symptoms either before or after the test. This suggests that either 22% of ‘cases’ are completely asymptomatic or the test has a really bad false positive rate - and bear in mind these people are selected for testing because they are considered higher risk. My guess would be a bit of both - but more research is required.
Doctor: Your test result is back; I’m sorry to say it looks like you have cancer.
Patient: Oh no! Could the test be wrong?
Doctor: We’ll do more tests of course, but the tests are only wrong about 1 time in 100.
Patient: So there is some hope that it’s not cancer then?
Doctor: You must try to prepare yourself for a long battle.
At first glance, a false positive result (the test says the person has the bug but actually they don’t) does not seem as bad as a false negative. Surely, the worst that can happen with a false positive is that the person has to self-isolate for a few days when they actually didn’t need to? However, the impact of false positive results has huge implications for policy making and epidemiology:
Imagine you have a FICTIONAL diagnostic test that is 99.5% accurate for a FICTIONAL bug. You test 1,000 sick people who you think may have the bug (but unknown to you only 800 (80%) actually do have it). 99.5% of the tests on the 800 who do have the bug come back positive = 796 +ve, 4 -ve. 99.5% of the tests on the 200 who do not have the bug come back negative = 1 +ve, 199 -ve. Overall 797 positives, 203 negatives. Good, that’s very close to the actual 800:200. The 797 go into isolation to reduce the chance of spreading it to their friends and family. It’s a bit of a shame about the 1 person out of that group being isolated unnecessarily but 796:1 is not bad, is it? Success!
Because of the above success you decide to start testing random selections of the population. You start by doing 10,000 tests per day. A shocking 6.44% of the tests come back positive. 644 positives, 9,356 negatives. The 644 self-isolate. Disaster! 6.44% of the population have the bug!
You ramp up testing to 100,000 random tests a day. You get 6,440 positives - the headline writers report a massive increase on the previous figures - but actually it’s the same percentage of the tests: 6.44%. The 6,440 self-isolate. Day after day you continue testing new batches of people, something (perhaps it’s a result of all the people you’ve instructed to self-isolate), begins to drive the percentage of infected people down.
You continue testing at 100,000 tests day after day. Eventually you get down to 6,242 positives. The 6,242 self-isolate.
You continue testing at 100,000 tests day after day. Eventually you get down to 3,866, then to 1,490, then to 896 positives. Each positive group begins self-isolation. It looks like you’re winning this battle.
In an Herculean effort you ramp up testing still further to 500,000 tests a day. You get 4,480 positive results. The headline writers start talking about a second wave - they don’t want to report that testing 5x as many people detects 5x more cases. The 4,480 begin self-isolation.
You keep pushing on, day after day: The figures slowly come down to 3,490, then 3,094, then 2,698 and after many days of effort you get it down to 2,500 positive results. You keep trying, but no matter what you do you can’t seem to drive this bug below 2,500 new cases per day… Has the bug developed resistance? Mutated? Are the positives breaking self-isolation? Are you being sabotaged by enemy agents deliberately spreading the disease? Perhaps it’s something being put in fast food? Or perhaps the delivery drivers are to blame? Are we doomed to have this bug with us forever?
In the FICTIONAL example above what has happened is that a 99.5% accurate test is far too inaccurate for a disease which is only present in a small percentage of the population. The lower the actual prevalance of the disease the more accurate the test must be to be of any use.
| FICTIONAL | Tests/day | Number +ve | False +ve | Detected % | Actual % | False +ve % |
|---|---|---|---|---|---|---|
| Sick | 1,000 | 797 | 1 | 79.70% | 80.00% | 0.13% |
| Random 1 | 10,000 | 644 | 47 | 6.44% | 6.00% | 7.30% |
| Random 2 | 100,000 | 6,440 | 470 | 6.44% | 6.00% | 7.30% |
| Random 3 | 100,000 | 6,242 | 471 | 6.24% | 5.80% | 7.55% |
| Random 4 | 100,000 | 3,866 | 483 | 3.87% | 3.40% | 12.49% |
| Random 5 | 100,000 | 1,490 | 495 | 1.49% | 1.00% | 33.22% |
| Random 6 | 100,000 | 896 | 498 | 0.90% | 0.40% | 55.58% |
| Random 7 | 500,000 | 4,480 | 2,490 | 0.90% | 0.40% | 55.58% |
| Random 8 | 500,000 | 3,490 | 2,495 | 0.70% | 0.20% | 71.49% |
| Random 9 | 500,000 | 3,094 | 2,497 | 0.62% | 0.12% | 80.70% |
| Random 10 | 500,000 | 2,698 | 2,499 | 0.54% | 0.04% | 92.62% |
| Random 11 | 500,000 | 2,500 | 2,500 | 0.50% | 0.00% | 100.00% |
If you consider that ordering many people to self-isolate unneccesarily is harmful then you should look closely at the ‘False +ve’ column in the table above. From the ‘Random 6’ group onwards you have more false positives than real positives and of course, from ‘Random 11’ you only have false positives.
You might think that the FICTIONAL example given above is too unrealistic - and you’d be right, but not in a good way: Unfortunately, in the real world, the false positive rate of Covid bug tests is not known for sure but has been estimated as 2.3%; far higher than the 0.5% used in the FICTIONAL example. The prevalence of positive tests in the people being tested is around 0.5%, well below the estimated false positive accuracy figure for the test - and bear in mind we are still predominantly testing people who report feeling unwell, their contacts and people who come into contact with many other people (medics, care workers etc). Believe it or not the only realistic bit in our FICTIONAL example is doing 500,000 tests per day. We desperately need more accurate tests… and more research.
Doctor: Your test result is back; it looks like you have the Coronavirus.
Patient: Oh no! Could the test be wrong?
Doctor: We’ll do more tests of course, but the tests are only wrong about 80 times in 100.
Patient: That’s terrible!
Doctor: No, not really, most people get over it in a couple of weeks.
There is now a push to test random samples of the population in the UK (up to now we’ve been testing sick people, people who care for them and people who interact with a lot of vulnerable people). This is good because it is more research - but any results must be treated with extreme caution.
The other type of test is an ‘antibody test’. This is a test to see if a person has been infected in the past and developed an immune reaction to the bug. Low-quality tests are available for the general public to buy and have caused worry among The Royal College of Pathologists - presumably because they may give too much reassurance to the general public who may then stop following the government advice. If the test is too inaccurate (false positives or negatives) then clearly it’s not fit for purpose and should not be on sale. If having had the bug in the past does not protect an individual from catching it again and/or passing it on again then the concern may be justified - but that would mean the bug behaves differently to most other bugs. However, the vast majority of people who test positive with such a test will probably think ‘when did I catch it?’ and ‘was that the nasty cold I had back in February?’ - which the test can’t answer, of course. There is a little evidence that having antibodies to the bug does indicate some immunity but as always, more research is needed to see how long any immunity lasts.
Doctor: Your test result is back; it looks like you’ve had it.
Patient (crying): Oh no!
Doctor: What are you crying for?
Patient (angry): Your bedside manner is rubbish! That’s a hell of a way to break the news.
Doctor: Eh? No, you misunderstand: You’ve had the Coronavirus and you didn’t even notice.
There is at least one other major problem with these antibody tests: People develop antibodies as part of their adaptive immune response - ie after a bug gets in and their immune system learns how to fight it off. However, people also have an ‘innate’ immune system which can react immediately as soon as a bug is detected. To stretch the vampire analolgy (possibly beyond breaking point) their body’s cells just know not to invite the bug in. Under these circumstances, there may be virus particles on the surfaces of someone’s throat or nose but no actual infection of cells and consequent disease. In other words, the person is immune, and is not generating new virus particles but tests positive for the presence of the bug and negative for antibodies. Much more research is needed.
Testing technology
On 17 Sep the BBC posted an article about a wall-mounted monitor which samples the air and sounds an alarm if the bug is detected… Just think about that for a moment. The creation of this device recognises the fact that the bug is free floating in the air - just like most viruses. This means that almost anything could have virus particles contaminating their surface - for example a person’s tonsils or nasal passages when taking a swab for a more standard test. This would help explain false positive results in standard tests - but not what to do about them.
On 18 Sep the BBC posted an article about a new shoebox-sized device which can provide coronavirus test results in 90 minutes. In the article the new test was compared with existing laboratory tests: ‘If the lab tests said the patient was free of the virus, so did the rapid test. If the lab tests said the patient had the virus, the rapid test agreed 94% of the time’ - or to put it another way: The rapid test disagrees with 6% of the laboratory positive results. Perhaps this means that the new test has the same or better false negative-, but perhaps a better false positive accuracy? We can hope.
Restrictions - Erosion of liberty.
On 30 March 2020 former UK Supreme Court judge Lord Sumption had a bit of a rant during an interview on the BBC radio program ‘World at One’. In the interview (transcript here) he stated that the new rules and regulations marked the UK’s ‘hysterical slide into a police state’.
So what was he on about? The UK parliament has passed laws allowing the government to take drastic action. Schools, colleges and places of worship were closed from 20 March and from 24 March shops which the government deemed ‘nonessential’, pubs & restaurants and personal service premises such as hairdressers and barbers were closed with a mantra of ‘Stay Home, Protect the NHS, Save Lives’. Nonessential businesses have to close their premises and staff in ‘essential’ businesses and organisations and shoppers in those shops which are allowed to continue trading are required to practise Social Distancing which means remaining 2 metres away from everyone else. Workers are to work from home if possible - and if not, to stay off work. The ‘Stay home’ element is reinforced with a few permitted reasons to be out of your home:
- shopping for basic necessities, for example food and medicine, which must be as infrequent as possible.
- one form of exercise a day, for example a run, walk, or cycle - alone or with members of your household.
- any medical need, including to donate blood, avoid or escape risk of injury or harm, or to provide care or to help a vulnerable person.
- travelling for work purposes, but only where you cannot work from home.
I’m not the only one I’m sure, but I never expected to see UK workers issued with Travel Permits by their employers in case they were challenged by police while travelling to work (I have a collection of them). I’m actually astonished at the level of compliance from the UK public.
It’s certainly not just the UK that has done this. Some countries have tighter restrictions than others and some started imposing restrictions sooner or later than the UK. Some, particularly those with a high percentage of armed citizens, are finding it difficult to maintain restrictions.
We now see warnings that having imposed restrictions on our liberty, our governments may try to not lift some of those restrictions once the crisis is past. ‘For the good of the people’, of course. There have been reports that the governments of Russia and Turkey, for example, have taken the opportunity to reserve greater power for themselves on a permanent basis. Goodness knows what liberties have been eroded under even more oppressive regimes such as Iran or North Korea. It will probably take years to find out.
Community transmission
(Norovirus on cruise ships, Diamond Princess)
Masks
After much debate and pressure from politicians in other parts of the UK, on 24 July wearing ‘face coverings’ in enclosed public spaces such as shops became mandatory in England. There are a few exemptions from wearing a mask and many premises and police forces have indicated that they will not challenge non-wearers. To try to boost compliance, the public messaging around this focuses on the protection of others (by you wearing a mask) backed up by fear-mongering about the severity of the disease and prevalence of the bug (in week ending 24 July (Week 30) overall deaths in England and Wales were 1.8% below the five-year average). To be helpful the UK government has issued a guide to making reusable masks out of old shirts or pillowcases. The Terence Higgins Trust has even issued guidance on wearing masks while having sex though I hope that advice is not intended to apply to enclosed public spaces.
The ‘science’ (such as it is) behind the mask debate hinges on whether the bug is transferred from an infected person with the virus particles suspended in gross droplets of body fluids (eg spray from coughs and sneezes) or just by being expelled on the breath or in sweat. No reasonable amount of cloth or fibre can filter virus particles out of air - to be effective such a filter would have to be so fine as to prevent the wearer breathing. Cloth masks would be no substitute for Hazmat suits which either have an air supply hose or tank or use a filter with a pump to force air through it.
Much discussion has swirled around the concept of infected people being able to pass on the bug before they experience any symptoms (if they ever do experience any symptoms). If this is true the bug can be passed on (without coughs or sneezes) just by being exhaled - and inhaled by someone else. Masks cannot help if this is true.
Some people object to wearing masks because their glasses steam up and some other people see this as a trivial inconvenience; but some glasses-wearers really can’t see well enough if they have to remove their glasses or can’t see through them. Aside from this the effect does highlight an important point: what is it that is condensing on their glasses? The answer, of course, is it’s the moisture from their breath and everything that’s carried on it. Ordinary masks can not prevent your breath from circulating around you and condensing on cooler surfaces.
If masks are there to prevent spray then there is a little merit in them. Certainly, if you cough or sneeze while wearing a mask, it will catch many of the larger droplets on the fibres of the cloth. However, some of that matter will be transferred to your hands when you take off or adjust your mask. The same is certainly true about coughing or sneezing into a tissue, but normal behaviour is to then dispose of the used tissue rather than continue breathing though it - and among more civilised people it is then usual to wash your hands. In the normal course of events matter from our coughs and sneezes often collects on our hands and transfers to other people’s hands via the things we touch. If infected matter is transferred in this way then people often infect themselves by touching their face and/or eyes (for example while adjusting their mask or cleaning their glasses). So does mask-wearing increase or decrease the likelihood of spreading the Covid bug? More research is needed.
Given the relative size of virus and some smoke particles (see above) it is worth noting that if it is possible to smell smoke or someone’s scent or body odour while wearing your mask then it is certainly not able to keep viruses out (or in).
It would be trivial to claim exemption from mask-wearing in the shops I go to. There are usually some people there not wearing masks and I assume that they are exempt for some reason. So do I wear a mask when I go shopping? Yes, even though I think it is useless (possibly detrimental) in preventing the spread of the bug among the people around me. There are a few reasons I wear a mask:
- I’ve been told to do so by people in authority. Although I think they are wrong it is not such a huge inconvenience to me (even though I wear glasses) that I will break the rules.
- If other people find a measure of reassurance in me wearing a mask then I’m happy enough to do that for them. Again, I think they’re wrong to be reassured and even more wrong to be frightened in the first place. Rather amusingly I have noticed that wearing a mask sometimes makes me cough - which quite probably makes people feel less reassured.
- I don’t think it will make any significant difference (positive or negative) to the overall spread of the bug in the long run. So I’ll go with the flow.
However, I have certainly found that mask-wearing interferes with my previously usual shopping habits:
- I’m a bit deaf and I now realise just how much benefit I get from seeing people’s lips move when they speak to me.
- It’s difficult to work out whether someone is smiling or annoyed - especially if their glasses have steamed up. Mistakes can happen.
- I have not gone into a shop to browse for several months. I only ever go with a shopping list. I do still make impulse purchases but I don’t go into a shop to gain inspiration for a project. In the past I’ve gone into a home improvement store to buy a piece of timber and come out with ideas to revamp my loft space - that’s just not happening these days. If many people behave like this the economy will not recover quickly - but I’m saving a fortune.
Proponents of masks often point to the medical professions for justification of mask wearing:
- Surgeons usually wear masks while operating. Yes, to prevent gross matter/droplets (sweat, dribble, dandruff, sneezes etc) falling from them into open patients and to protect themselves from gross matter spraying from the patient when the surgeon is operating things like a bone-saw. Note: Surgeons never, ever, reuse such masks.
- Doctors, dentists and nurses often wear masks when examining or treating patients. Yes, when was the last time you got so close you could put your fingers in a stranger’s mouth in the supermarket? (Please don’t try this).
- Medics don’t expect masks to filter free floating virus particles out of the air. For that they would use hazmat suits.
I’m very concerned that sometimes I see people in open public spaces (eg in a park) wearing face masks. I assume they don’t wear these masks at home but they seem to think that the risk is greater in the open air. Perhaps at home they have very fine net curtains which can stop the viruses floating in the air from entering or leaving their homes? More seriously I guess they just generally feel safer at home. It’s sad to see such frightened people.
I came across this article. I strongly disapprove of the head teacher’s stance. I’d better not say any more…
The WHO issues and updates guidance on mask-wearing - the latest advice (issued 5 June 2020) contains the following (I’ve omitted the references but you can find them by following the above link):
| Guidance on the use of masks for the general public | |
|---|---|
| Available evidence | |
| Studies of influenza, influenza-like illness, and human coronaviruses (not including COVID-19) provide evidence that the use of a medical mask can prevent the spread of infectious droplets from a symptomatic infected person (source control) to someone else and potential contamination of the environment by these droplets.(54, 55) There is limited evidence that wearing a medical mask by healthy individuals in households, in particular those who share a house with a sick person, or among attendees of mass gatherings may be beneficial as a measure preventing transmission.(41, 56-61) A recent meta-analysis of these observational studies, with the intrinsic biases of observational data, showed that either disposable surgical masks or reusable 12–16-layer cotton masks were associated with protection of healthy individuals within households and among contacts of cases.(42) |
-
…from a symptomatic infected person… In other words, ‘people who are coughing badly or have a fever’. In which case they shouldn’t be going shopping. The same would be true if they thought they had a ‘flu.
-
…mass gatherings… Sports matches, political rallies, protest marches (same thing) or raves - not ‘going to the grocery store’.
-
…disposable surgical masks… Does anyone imagine that the disposable masks you can now buy in the supermarkets are ‘surgical masks’? Sure they look vaguely like the things we see in films - but ask yourself would the NHS buy them for use by surgeons?
-
…12-16-layer cotton masks… Bandanas or masks made of three layers of old shirt cloth are not really going to make any difference.
To be honest I’ve engaged in selective quoting of the WHO guidance. The document contradicts itself in different sections. To find out more you’ll have to actually read it.
There are certainly reasons to wear masks in some circumstances but going shopping is not one of them. However, one really good reason to wear a mask is to defeat the egregious abuse of face recognition cameras in some shopping malls.
Education qualifications
Because of the lockdown it has not been possible to conduct education Examinations in Summer 2020 and so school qualifications have been awarded based on teachers’ assessments of how well or otherwise a student was expected to perform had they actually sat a properly controlled examination. Examination boards found that many more students were assessed to perform better than students from the same school actually had performed in previous years (this, of course, has absolutely nothing to do with the fact that parents assess the performance of schools on number of students achieving certain grades). To try to address this problem a formula was created to deflate what might be inflated grades. Yes, they tried to apply statistics to individuals - statistics is inherently about groups not individuals. An examination is very much about the individual’s performance on the day. The application of the formula was deemed to be so unfair it was rapidly abandoned but not before many people got very upset. More thought is being given to this problem to try to get the ‘right’ students into further education and to award grades that prospective employers might be able to place some faith in.
I don’t know about anyone else, but if I were looking for an employee and was faced with a young person with a qualification in Maths from 2020 and another with the same qualification from 2019, I’d trust the latter certificate to be more realistic. That said, the simplest approach would be to give a short test at interview to see which person performs better - and otherwise ignore the ‘qualification’. Hey, what a brilliant idea! Further Education establishments could give tests! What should I call this… I have it! Entrance Exams! Remember, that was my idea first. What? Already been done? Bah.
The teachers who were required to give their students assessed grades must have felt enormous pressure. Mark bright little Johnnie down because although he’s bright he spent too much time pratting about at the back distracting Mary? What about that girl that you don’t actually like very much? Is she bright or just a smart-arse? How to make sure you’re being fair to her? Also, I wonder who gave that tough lad a ‘pass’ in Maths and do his mates know where his Maths teacher lives?
The hand-wringing that is going on trying to be ‘fair’ to students is sickening. The unfairness stems from when the country trashed three months of their education and scrapped their opportunity to demonstrate how well they’d learned.
Summer 2020 education qualifications will go down in history as bogus. Students graduating to further education or employment this year will need to be assessed separately by colleges and employers.
How do we get out of lockdown?
The UK civil service has done an impressive job in implementing the emergency financial measures ordered by the government. Among many other things these measures include making payments to businesses to partially cover employees’ pay while productivity is at a standstill and cutting or delaying the collection of taxes. Businesses are being protected from having to pay out money that they are not receiving.
If you think about it, these employees are being paid to do nothing - and the employers too - at a time when the income for the government (local as well as central) has dried up. The government is paying out money that it does not have and is not receiving in taxes. It risks going bust.
Having applied the economic brake so abruptly it will take time and energy to get the economy rolling again. If all the work restrictions were lifted tomorrow and the payments ceased at the same time many businesses (parts of the economy) would go bust and cease trading. Payments will have to taper off as procuctivity gradually improves - but some businesses will still not survive the process.
What about the social aspects? During lockdown we have been told to stay 2m apart. So will it become OK to walk past someone in the street the day after lockdown is lifted? What about greeting people with a handshake? Is that gone forever? What about the habit of the French to greet each other with a kiss (or several) on the cheek? Will it overnight become acceptable again to jostle for a place at a bar to get drinks for your friends? Who will be working at these bars?
The second wave - or ‘Winter’s coming’
Many media outlets are warning about a ‘second wave’ of the bug and many are urging our politicians to impose tighter restrictions to ‘prevent’ this happening. Some rightly point out that ‘influenza-like-illnesses’ spread more easily in the Winter months and so predict dire consequences for the Northern hemisphere Winter 2020/2021. Usually in the 4-months of December to March each year more people die in England and Wales than in the 4 months preceeding or following. ONS measures and refers to this as ‘Excess Winter Mortality’. This excess mortality is made up of accidental deaths (slipping on ice, road accidents), hypothermia (‘freezing’ to death) and other seasonal causes - and the majority are due to ‘influenza-like-illnesses’ (ILI). Since the 2000/2001 Winter (after ‘flu vaccinations for over-65’s were introduced) the excess deaths have been about 0.05% of the population on average - which corresponds to about 30,500 deaths out of the current population. These deaths are usually among frail and/or elderly people with other health problems - just as with Covid-19. I would contend that it does not matter whether someone dies of pneumonia caused by ‘flu or this new bug; what matters is how many die of either.
The UK government’s Covid-19 ‘dashboard’ site shows dramatic graphs of an increase in ‘cases’ (actually positive tests) and deaths in September/October…

Data downloaded from UK Government Covid-19 dashboard 22 Nov 2020, aggregated for England and Wales only. Note the almost complete lack of correlation between ‘cases’ and deaths.
But the ONS weekly stats tell the same story in a different way.

Not quite so terrifying is it?
There can only be a ‘second wave’ of deaths in those countries that have managed to stop a ‘first wave’ of deaths among a reservoir of frail, vulnerable people. If there is no such reservoir then they will see a normal rate of death among people as they become frail and vulnerable over time. Some of these deaths will be attributed to Covid-19.
Emperor’s new clothes? Boy who cried ‘wolf!’.
The economic impact
There was once a brilliant pioneering surgeon who invented artificial heart valves for patients who had damaged ones. The trouble was it was very fiddly to cut the failed valve out and sew the new one into place. The process was far too difficult with the heart beating.
This clever chap realised that if he could cool the patient right down he could stop their heart for 30mins without the patient suffering any brain damage. So if he could perform the surgery in 30mins on a stopped heart he should be able to get the job done. He practised how to do this very fiddly surgery on animal hearts he bought from the meat industry and got his time down to below 30mins…
He knew the procedure was risky so he carefully selected a patient and explained what he wanted to do and emphasised the huge benefit for the patient. On the day of the surgery he cooled the patient right down and the heart stopped and he started the operation. Things were a little more fiddly than during his practice sessions and he began to fear that he would not finish inside 30mins. The pressure mounted as the clock ticked on and then finally… success! He finished with just seconds to spare. ‘I’ve done it!’ cried the surgeon, ‘Now, who knows how to start this guy’s heart?’
We are currently in the middle of one of the most extreme economic experiments ever conducted. No government or group of governments has ever deliberately closed down their economies with the intention of restarting them later. The Chinese ‘Cultural Revolution’ and Cambodian ‘Auto-Genocide’ did trash their economies - but their revolutionary governments certainly had no intention of allowing them to restart in anything like the same form as before.
If such an economic shutdown has never been attempted before, then it follows that neither has the required economic restart.
Governments are spending money and making binding spending commitments to try to stop the collapse of businesses which they have forced to close. Once this crisis is past our governments will need to balance the books and raise taxes to pay for this. In the long run governments can only spend what they can raise in taxes - and, at least in the UK, they only take a cut of money when it moves (eg NI contributions when an employer pays an employee; income tax and NI (again) when an employee receives pay; sales tax (VAT) and other consumption ‘duties’ such as alcohol and fuel tax when a person buys something; tax on interest earned from savings; capital gains tax when a person sells something for more than they paid for it; inheritance tax when a person dies and leaves money to beneficiaries; corporation tax when a company makes a profit). Taxes will have to go through the roof.
The UK government has borrowed a truly staggering amount of money to pay for the lockdown. At one stage ONS reckoned that in April 2020 the UK government borrowed more than it had ever borrowed before in a single month - but later reduced the estimate somewhat - but in May 2020 they borrowed even more. For the first time in nearly 60 years (since 1963) the UK’s debt exceeds its GDP. 1963 saw the UK finally bring the debts the country had incurred in fighting and surviving World War II (which had ended 18 years before that) down below the total amount of wealth that our people generate in a whole year.


On an individual or family level anyone who has ever taken out a mortgage or long-term loan to buy an expensive item should realise the interest payments on the loan can mount up to a significant chunk of what was originally borrowed (with a 25 year mortgage at 3.5% you can end up repaying 50% more than you borrowed). Borrowing to fund big-ticket items like a house or car is one thing, but if you find yourself borrowing to pay the regular bills then you’re in serious trouble and in danger of sliding into poverty. Taking out new loans to help you pay off existing loans will not help in the long run - it perpetuates the problem. Owing big money to the loan-sharks is never a good idea.
Because of the duration of government-level loans these usually bind future governments into paying them off. If a government issues a 20-year bond then all subsequent governments during that 20 years will have to make the interest repayments and whoever is in power 20 years later will have to pay it back - and if the country can’t afford it, they have to issue a new bond and make the terms attractive enough (compared with other countries’ bonds) that the money-lenders will buy them. Because of the way bonds work, a government can attempt to buy some of them back part-way through the term and thus reduce the overall amount of debt and reduce the size of the final repayment. However, many governments won’t do this as the need to keep the elecorate ‘sweet’ by spending more on them outweighs long-term fiscal prudence. A country whose government incurs more and more debt without ever reducing the total amount will develop a bad credit rating and find that only high-interest loans are available - which means that big-ticket development projects (like major roads, railways, hospitals, stadiums, fighter jets etc) become unaffordable. If a country’s government cannot make a repayment (because it can’t sell or won’t issue new bonds) then it might default on the final payment (effectively declaring bankruptcy) which will put it in an even more difficult situation. Venezuela (2017) and Lebanon (2020) are recent examples of such a financial default - the money-lenders won’t want to buy bonds from those countries any time soon.
Governments all around the world are trying to borrow money to meet the immediate needs of their country. The money-lenders don’t have cash stuffed in their matresses or sitting in bank accounts - it’s invested in other countries or businesses or property or bonds. To get the money-lenders to lend to them governments need to promise a better rate of return than they are currently getting and/or a lower level of risk of losing on the deal. To invest in new government bonds the money-lenders must first sell whatever they are already invested in in order to release the ‘cash’ to buy the new bonds - and the urgency of selling quickly drives down the price they get and introduces volatility in the market. So the new deal has to be made even more attractive to persuade the money-lenders to invest. But what are the money-lenders selling to invest in the new government bonds - property and businesses that need the investment money to grow and employ more people. Worldwide government borrowing directly hits investment in businesses which in turn can drive up unemployment.
Don’t get carried away with the idea that money-lenders are bad. Without them governments could not afford most infrastructure projects. Many people’s future pensions (even state pensions) are backed by them and most home-owners couldn’t afford to buy a home without a mortgage. Of course, as an individual, you could choose to rent your home instead, but someone will own the home you live in.
Many people’s livelihoods will be wrecked by the lockdown (there are reports that 600,000 people have already lost their jobs in the UK) and this will likely have an effect on their long-term well-being. In less well developed parts of the world governments will not be able to provide a financial safety net for workers laid off due to the downturn in the economy. For example there are already reports of clothing manufacturers laying off workers in India, Bangladesh and elsewhere because their businesses are on the point of collapse - first due to production difficulties because of shortages of cloth to make the clothes and now due to a massive decrease in buying the finished products in the West. How are these guys going to afford the food and health care that they need just as much as anyone in the developed world?
Some will be outraged at the idea of worrying about how we’re going to pay for this at a time when people are dying. I would counter with a few points:
- It is quite common for people to refer to their employment as their ‘livelihood’ - there’s a clue in that word. It is well known there is a strong correlation between poverty and low life expectancy. Destroying employment by preventing people from working, destroying the aviation and tourist industries, closing most shops, theatres, restaurants, bars and damaging kids education by closing schools and colleges, will push more people into poverty which will (statistically) result in earlier death for some. Incurring more and more debt will require an ever larger slice of the country’s wealth (GDP) to pay the interest and will drag down the amount spent on welfare support for disadvantaged people. Average life expectancy in the UK is high compared with many other countries, but the disparity between the wealthiest and poorest is significant.

-
At a smaller scale (family/individual level) shutting down the economy means that poorer households are disproportionately affected by the worldwide lockdown. So-called ‘white collar’ workers are far more likely to be able to work from home than those who work producing goods or providing services for others and are therefore less likely to be laid off during the lockdown. And that is just for regular employment; gig economy workers are particularly badly hit; not to mention grey economy workers (cash-in-hand cleaners, gardeners, fruit pickers etc). You might have difficulty finding sympathy for the latter group but it would be immoral to leave them starving. Lower wage earners are more likely to work in gig economy or zero-hours contract jobs which provide no guaranteed income during the lockdown (for example, if fewer people are travelling, fewer taxi- and bus-drivers are needed). Also, people from poorer households are less likely to have a good credit rating and so, if they need or want to take out a loan, will get less favourable terms from money-lenders. Even large, well-established lenders such as banks and building societies with published interest rates are likely to demand greater insurance against defaulting on repayments of any loan which makes it more likely that these people may take out riskier loans from unregulated (illegal) lenders. All of this is the effect in well developed countries like the UK which can just about afford to have a 3 month economic pause; it’s far worse in developing countries.
-
We seem to have lost sight of the original aim: Flatten the peak! Protect the NHS! (ie prevent the number of cases from exceeding the health service capacity at any one time). I don’t recall the aim ever being to eradicate the disease completely - the only disease mankind has ever managed to eradicate is smallpox; even polio still keeps coming around from time to time. The UK commissioned a few ‘Nightingale hospitals’ to boost NHS capacity - and more-or-less didn’t use them. The UK health service as a whole was not overwhelmed though ICU staff worked wonders and were pushed beyond what was thought possible and are suffering as a result. Even in the worst ‘predictions’ (and there were many) the epidemic was never going to develop into an existential threat to the UK. However, now the peak has apparently been flattened the emphasis seems have shifted to not let anyone else catch it ever which I very much doubt is achievable. I’m not at all convinced that the lockdown has even slowed the spread of the disease in the slightest - or that it would have done so if imposed earlier.
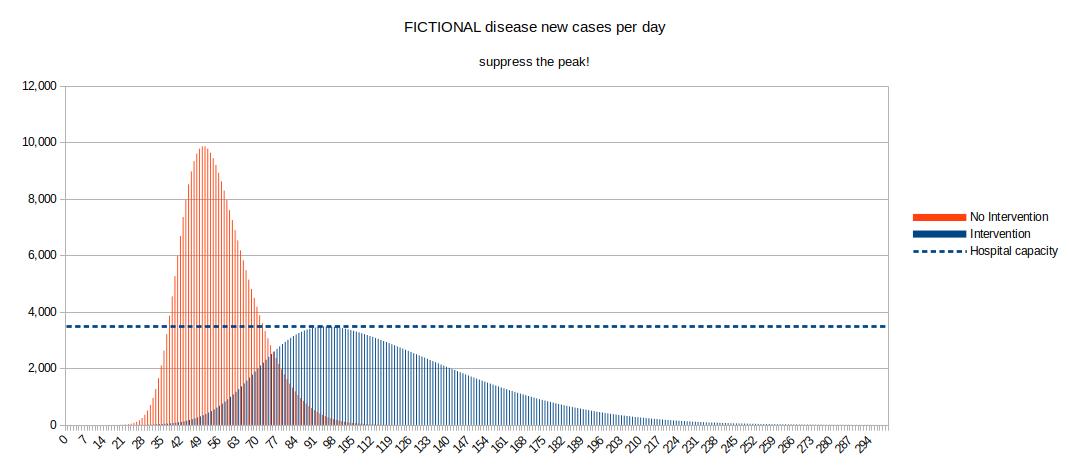
The graph (which uses FICTIONAL ‘data’) demonstrates the concept behind the original declared aim of the UK government in introducing lockdown (the ‘Intervention’). The No-Intervention and Intervention examples each represent 60,000 new cases but the Intervention example never exceeds hospital capacity. Note that the course of the disease in the population continues for a lot longer in the Intervention example. Getting the timing of the intervention right requires a good understanding of how infectious the disease is, which is impossible with a new virus. In the example given the intervention (lockdown) was imposed before any cases were seen - which again, would be a good trick if you could do it.
‘We haven’t seen any cases yet but you must all stop work and stay at home’ - Yeah right. That’ll work. -
Another approach is to take it to absurd extremes and see where people will draw the line:
- A friend will die unless they get treatment costing one hour of your wages. Will you pay?
- A friend will die unless they get treatment costing one day of your wages. Will you pay?
- A friend will die unless they get treatment costing one week of your wages. Will you pay?
- A friend will die unless they get treatment costing one year of your wages. Will you promise to pay?
- A friend will die unless they get treatment costing five years of your wages. Will you promise to pay?
- A friend will die unless they get treatment costing ten years of your wages. Will you promise to pay?
- A friend will die unless they get treatment costing twenty years of your wages. Will you promise to pay?
- A friend will die unless they get treatment costing your wages for the rest of your life. Will you promise to pay?
- A friend will die unless they get treatment costing your child’s wages for the first year of their working life. Will you make that promise that they will pay?
- A friend will die unless they get treatment costing your child’s wages for the first ten years of their working life. Will you make that promise that they will pay?
- A friend will die unless they get treatment - you need to commit yourself and your children to slavery until the debt is paid. Will you sign that contract?
Where on the above scale do you draw the line (if at all)?
- Someone the other side of the world who you don’t know needs treatment.
Is the line in the same place?
Not everyone will draw the line at the same point though I do hope nobody was prepared to indenture their children. Others will point out that in the scenarios above the treatment was available but that the person or organisation who had it was ‘holding us to ransom’ - and so absolve themselves of any blame. Perhaps they will even persuade themselves that they would be justified to seize the treatment by force. They will completely ignore any relative need or scarcity value or amount of time or effort which went into creating the treatment.
Of course, this is not how treatment for your friend would really be paid for in most parts of the developed world. In the UK with Covid-19 for example, your friend would be just one of thousands of people and their treatment will be provided by the NHS which will be paid for by taking money in taxes (perhaps from your wages). If you think you don’t pay tax because you earn less than the income tax threshold then wonder instead why VAT (sales tax) is charged at 20% on many goods you want to buy. In other countries you will be paying your medical insurers including the medical insurer of last resort - your government (whether local, state, nation or all of these).
We all require our governments to take on projects which are beyond us as individuals. For example I could never be a high court judge or organise the Defence of the Realm or build a high speed rail line from London to Birmingham but I expect my government to make arrangements for these jobs to be funded (OK, I didn’t actually want HS2). So how much of your money are you prepared for your government to spend to ‘save just one person’s life’? Given that everyone will die eventually would it make any difference to you if the person being ‘saved’ is a baby, a child, a young parent, retired, 80, 90, 100 or more years old (sorry if you feel I’ve unfairly excluded anybody from my list of examples)? I sincerely doubt that a majority of 100-year-olds would encourage their great-grandchildren to spend 20 years wages to ‘save’ their lives. Now scale that up: how much are you prepared to pay to ‘save’ thousands of lives?
Governments do borrow money to achieve worthy things. For example in 1835 the UK government borrowed £15m (equivalent to £1.9bn in 2020) in order to fund the abolition of human slavery in the British Empire under the terms of the Slavery Abolition Act of 1833. Perhaps interestingly the remainder of this loan was finally paid off in 2015 during the Cameron premiership. I wonder if William Lamb (Prime Minister in 1835) ever imagined it would take 180 years to clear the debt?
‘Did’, ‘Probably did’, ‘Possibly did’, ‘Could have’, ‘Might have’, ‘Didn’t’…
…and their unwelcome cousin ‘Would have’.
In almost any branch of science researchers are trying to find out more about their field of interest. Many PhD theses are written on research expanding mankind’s knowledge in very specific and narrow ways. For example, one now famous person’s doctoral thesis was titled ‘Properties of expanding universes’ and examined the implications and consequences of the theorised expansion of the universe, before concluding that galaxies cannot be formed as the result of early perturbations. The thesis is widely recognised to be flawed - but this recognition does not detract from the author’s fame; he was, of course, Stephen Hawking.
In almost any subject ‘The Science’ is never settled. Let’s take a simple example that (nearly) everyone can agree on:
‘The Earth orbits around the Sun’. There. The Science is settled…
What’s that? Oh yes, well really the Sun and the Earth both orbit about a common point which is not at the centre of the Sun but is still inside its surface…
What’s that? Oh yes, well the Sun doesn’t really have what most people would call a ‘surface’ but you know what I mean. It’s close enough…
What’s that? Yes, I know Einstein showed that actually the Earth continues in a straight line but that Spacetime is curved…
Don’t worry. The Science really is settled this time…
…but it never is.
It is often repeated that the UK government and other governments around the world ‘followed The Science’ in their decision making about the bug. However, there is no such thing as ‘The Science’ - especially when talking about the complexities of a new bug and the vagiaries of people’s behaviours when faced with it. What they mean is that they followed the advice of the scientists they trusted most. They may even have tried to take into account the many differing opinions among various scientists and followed what they thought would be a ‘least harm’ policy - but where ‘harm’ is necessarily an opinion based concept.
But how successful were our governments in minimising harm?
In the early 19th Century a mathematician called Benjamin Gompertz published a paper on estimating mortality among people. He was an actuary and his work was used by insurance companies to assess risk and set prices for Life Insurance policies. His work was expanded upon by others and the concept of the ‘Gompertz curve’ (or Gompertz formula) has found application in the statistics concerning biological processes from tumour growth through agriculture to epidemiology. His original work was based on the assumption that ‘a person’s resistance to death decreases as his years increase’ - which can be roughly re-phrased as ‘the older you are the more likely you are to die’. Who’d have thought?
Gompertz curves appear in many natural biological processes. If the progress of a biological process follows a Gompertz curve we can deduce that the conditions that drive the process do not change over the course of time - there are no ‘interventions’ in the process. A deviation from such a curve indicates a change in the conditions driving the process (for example the introduction of culling in a pest population or the application of weed killer or fertiliser in agriculture or the delivery of a vaccine during an epidemic). If there are significant deviations from the curve these can indicate the timing of changes to the conditions.
Early in the course of the epidemic in the UK, ONS began to include in their weekly datasets a daily cumulative count of deaths in England and Wales where Covid-19 is mentioned on the death certificate. If we plot these deaths against date we get something which looks very like a Gompertz curve - which is not at all surprising as this is a natural biological process.
If we ‘fit’ the daily death data (blue bars, right scale and red curve, left scale) to the closest mathematically correct Gompertz curve (yellow curve, left scale) the match is remarkably close (never further than about 1,000 above or below the curve, only about +/- 2%). Even though the red and yellow curves match closely we can measure what differences there are between them (green curve, right scale). If the differences varied randomly above and below zero then we couldn’t gain much knowledge (science) by examining them… but actually we can clearly identify trends and points where the observed death count abruptly begins to increase or decrease relative to the ‘pure’ mathematical curve. The dates of abrupt changes to the closeness of the match indicate when interventions (changes to the overall conditions driving the process) have had an effect - and whether that effect is an increase or decrease in the death count.

Notes:
- Just to demonstrate how stupid it is to extrapolate from too little data and/or to assume exponential when talking about an epidemic, I have included a best fit exponential trend line (the pale blue curve) based on the ‘first thousand’ (actually only 956) deaths up to lockdown on 23 March 2020 (mid-way through week 13 of the year). It shows no correlation with the reality beyond 23 March whatsoever.
- According to this extrapolation, before the end of 1 May (end of week 18, 39 days later) everyone in England and Wales would be dead.
- The ‘best fit’ (via non-linear least squares method) Gompertz curve (yellow curve) and therefore the differences (green curve) will change with each new weekly batch of data that is added to the dataset. If the curve changes significantly it will indicate a large change in the data added.
Click here for a slide show of charts comparing number of deaths known at the time extrapolated to best fit Gompertz curves for each week from week 14 to date. The first few deaths in England and Wales (barring one earlier outlier) occurred in the week ending 6 March (week 10 of the year, published 17 March), by which point there had been 7 deaths associated with Covid-19. At 3 April 2020 (week 14, published 14 April) we had seen 7,512 deaths and the best fit Gompertz curve extrapolated to 167k deaths. By week 15 (published 21 April; 15,750 deaths; extrapolation to 62.2k) or week 16 (published 28 April; 24,057 deaths; extrapolation to 46.2k) the extrapolations stabilise closer to what we now know to be reality (ie 5-6 weeks from the first few deaths).
So, how are we doing? From the green curve on the chart, dates of interest include 30 March 2020 (very bad), 18 April 2020 (good), 25 May 2020 (bad) and 20 September (bad).
The effects of any events take different amounts of time to show through death statistics; for example it might take some weeks for someone to die after catching a bug but considerably less time to die after (say) being bludgeoned about the head. If we have to wait for registration of the death this will introduce further delays. I’ve shown above that because we are using deaths as our measure (in this case actual dates of death where Covid-19 is mentioned on the death certificate) we have to allow for a lag of about 23 days between an intervention intended to reduce infections and a reduction in consequent deaths… And look at that! 23 days prior to 18 April 2020 is 26 March - just 3 days after lockdown. Hooray! The case for lockdown is proved!
But hold on. What’s that spoiling things around 25 May? It’s a much more gradual change but 23 days prior to that is 2 May. What happened around then? As far as I can tell there was no policy change or other significant event around the beginning of May but one milestone we do have is starting the sixth week of lockdown. I can’t prove it (correlation is not causation), but this looks to me like people beginning to rebel against lockdown - just as government suggested they would.
We might expect the various stages of lockdown easing to have a noticable effect in the stats:
- The ‘Stay at home’ policy was lifted on 17 May (23 days later is 9 June, week 24)
- pubs reopened in England from 4 July (23 days later is 27 July, week 31)
- masks became mandatory in shops in England on 24 July (23 days later is 16 August, week 33/34)
- children went back to school in early September (23 days later is around 26 September, week 39/40)
- ‘rule of six’ comes into force 14 September (23 days later is 7 October, week 41)
- local lockdown in large parts of NE England from 18 Sep (23 days later is 11 October, week 42)
The only visible effect on the death rate around those dates is a very minor drift after the kids went back to school. Waiting and watching for data from week 42 onwards when ‘rule of six’ and local lockdowns should be expected to bend the curve down if they have any effect at all.
But what about the elephant in the room? Yes, I’m now looking at 30 March 2020. Over just a few days the death rate changed from falling steeply away from the mathematical curve to rising sharply towards it. 23 days prior to 30 March is 7 March and the first seven deaths in England and Wales where Covid-19 was mentioned on the death certificate occurred between 2-7 March (apart from one outlier on 30 January) but I can’t see how a few deaths can ‘cause’ many more (this is not a war). I have a nasty feeling that what we’re looking at is something which had an effect in just seven days (far less than 23 days). On 19 March the NHS issued a policy document describing how to free up capacity in the hospitals:
| COVID-19 Hospital Discharge Service Requirement | |
|---|---|
| 1.4 Implementing these Service Requirements is expected to free up to at least 15,000 beds by Friday 27th March 2020 |
I believe the sudden increase in deaths (relative to the mathematical curve) starting around 30 March is directly due to the introduction of lockdown (23 March) and associated policies by the UK authorities - and specifically clearing the hospitals by the NHS policymakers (19-27 March).
Can we use the data to make any further deductions about the spread of the bug in England and Wales?
- As shown above, it takes an average of around 23 days from infection to death (for those that are going to die).
- First deaths were recorded in early March (apart from one outlier in late January).
- The infections leading to the first deaths must have occurred around 11 February (ie 23 days prior to early March); the UK’s first case was reported in the media on 2 February.
- The bug was therefore spreading more or less uncontrolled from 11 February (or before) to the 23 March lockdown (ie for at least 41 days).
- If the bug were spreading exponentially (see above) 41 days would be more than enough for the whole population to be exposed. The spread is not exponential, of course; it’s Gompertz.
- By 4 September, about 52,000 people have died out of about 60m population (0.09%). This is the minimum infection fatality rate (IFR). (IFR will be higher if fewer than the whole population of 60m people have been infected).
A few last points:
- The differences between the observed number of deaths and the mathematically derived curve vary by only about +/-1,000 deaths (~4%) over the whole time period (but do bear in mind that the parameters for the Gompertz curve were selected to provide the best fit for the data).
- It appears lockdown had an almost immediate negative effect (~2,500 more deaths over 21 days)…
- …and a later slower positive effect (~2,100 fewer deaths over 35 days)…
- …and the breaking and/or easing of the lockdown has had a much more gradual negative effect (~1,700 more deaths over 95 days).
- All these effects are small in comparison to the overall number of deaths (~52k) over the course of the epidemic so far.
- There is no sign of a so-called ‘second wave’ in the death stats (bear in mind the anticipated 23 day lag).
- As always, more research is needed.
So how successful were the governments of England and Wales in minimising deaths?
- Lockdown and social distancing seem to have had a small mixed effect on the death rate (bad, then good).
- Later measures such as reopening shops, pubs and restaurants and mandating masks in enclosed public spaces seem to have had no effect.
- Reopening schools has had a minor bad effect on the progress of the epidemic
- The progress of the epidemic shows no major deviation from what we might expect with no interventions at all.
‘Cases’ vs deaths
I’ve tried to use information from realiable sources throughout this post but I now find the need to refer to some very iffy numbers. I mean the number of ‘cases’ of Covid-19 as published on the UK government Covid-19 dashboard. It’s not that I think that the governments are making up these numbers - just that the definition of a ‘case’ of Covid-19 has become ‘provided a sample which tested positive in an RT-PCR test’. No disease symptoms - just a positive test; 357,010 positive tests. The actual death count is provided by ONS and is less open to change by shifting opinions; it is a more trustworthy number.

- If we assume that a proportion of the detected ‘cases’ lead to death then it follows that the peak in numbers of deaths recorded by ONS as mentioning Covid-19 on the death certificate should be preceeded by a peak in number of ‘cases’.
- Looking at the peak of ‘cases’ on 5 April and the peak of deaths on 10 April it appears ‘cases’ are confirmed around 5 days before death.
- On 9 September there were 10 deaths. Five days before, there were 2,284 ‘cases’ diagnosed (mid 7-day averages). The ratio of ‘cases’ to deaths at this time is about 219:1.
- To reach 52,421 deaths at 219:1 there must have been around 11.5m ‘cases’. This is about 19.1% of the England and Wales population.
- If 11.5m people have had the bug and only 357,010 people got tested then 11.14m people (97% of ‘cases’) didn’t get sick enough to seek a test.
- If only 19.1% of the population have had the bug and the lockdown was effective in limiting the further spread then there is the risk that more people will catch it and fall sick and/or die - the so-called second wave (or first wave for places like New Zealand). However, it looks like 97% of the infected won’t notice - perhaps a good tactic would be to take extra care of the other 3%?
- A case Fatality Ratio (CFR) of 219:1 (0.45%) is very high compared with the 0.1% for the Asian (1956-58) and Hong Kong (1968-69) ‘flu pandemics. This CFR seems unlikely to be true as the absolute death count (so far) is considerably lower than for either of those pandemics.
- Nobody imagines that all cases are being diagnosed. If they were:
- If self-isolation worked, the bug would have stopped spreading.
- CFR would have to be 14.7% - which puts it in the same league as many tropical diseases which are on the HCID lists (such as Lassa Fever).
- Perhaps the CFR is actually as low as 0.1% (where ‘cases’ are as loosely defined as above):
- To reach 52,421 deaths at 0.1% CFR we would have to have had 52.4m ‘cases’ which is 87% of the population and which is more than enough to reach that magical thing called Herd Immunity.
- If 52.4m people have had the bug and only 357,010 people got tested then 99% of ‘cases’ didn’t get sick enough to seek a test.
- Clearly we must be somewhere between these two extremes:
- CFR of 0.45%, at least 19% of the population have had it and 97% of cases didn’t get sick enough to need testing
- CFR of 0.10%, at least 87% of the population have had it and 99% of cases didn’t get sick enough to need testing
- If the CFR is 0.1% or below and/or 97-99% of people shrug it off and/or a large percentage of the population have already had it why are the emergency restrictions being maintained or strengthened?
So why did we lock down and why are we about to make the same mistake?
What will history say?
When this pandemic eventually blows over it will be impossible to say with certainty what would have happened if our governments had taken different actions but there will be any number of arguments batted back and forth to convince us of one analysis or another. There are already headlines predicting that one country will be hit harder than another, and attempting to explain why (UK cf Sweden cf New Zealand, for examples). If these predictions come true then the headline writers will say ‘I told you so!’. If the predictions do not come about then no doubt that will be because the powers listened to the warnings and changed policy. Predictions abound that the death toll for Covid-19 will be worse than for one of the various ‘flu pandemics in recent history - and at least one of these predictions will turn out to be correct (there you go, yet another prediction). In none of these cases did we shut down our economies - although to be fair, the 1918 world economy had already been trashed by the first World War. We left it to individuals to decide whether it was sensible to go to the pub, hang out with mates, work close to another person, travel on holiday, visit Granny etc etc.
Governments around the world have followed one another into crude, unnecessary, ineffective and outrageous overreactions (with the possible exception of the Wuhan City or Hubei Province government which led the way). Governments now find themselves in the embarassing situation of trying to reverse some of the controls they imposed without allowing their people to notice how little effect they had on the death rate. So they will substitute ‘wearing masks’ instead of ‘staying in’ and similar rules as token gestures of control.
Just to be clear:
- governments are not colluding or conspiring in this. No such conspiracy could remain secret for long (even the US National Security Agency can’t keep secrets); each government has its own sense of self-preservation. To admit they’ve been so catastrophically wrong would invite revolution - either at the ballot box or on the streets.
- 52,000 deaths in England and Wales (and similar proportions of other populations world wide) is not trivial, but it’s not unusual either. However, our UK governments’ response could not and did not make any significant difference to the death total. At best, it has delayed reaching that total (which was one of the original stated aims).
In the short term our current governments will claim that their actions and policies saved us or reduced the impact of the pandemic - or that they had to be ready ‘just in case’. If they had not done what they did it would have been a disaster or worse disaster. They will praise a majority for following their advice and denigrate a minority who flouted the rules. If the experts they listened to prove to be ‘wrong’ then they will claim that they took the best scientific advice available and that other experts did not get their message across adequately.
In the medium term our next governments (probably those currently in opposition) will claim that the current governments either overreacted or didn’t go far enough (or preferably both within the same speech). They will claim that their predecessors spent too much on the wrong things and too little on the right things. That they listened to the wrong experts and that they didn’t listen to their experts. They will claim that they would have done things better if they had been in power. When we see many of these sorts of claims pushing other news out of the headlines we can be confident that the worst of the pandemic is over.
Hindsight is such a wonderful tool - people really should use it far sooner than they do. Only in the future (10-20 years or more) will we get any disinterested perspective on the events taking place today. And we will still owe the money-lenders and be repairing the economic damage.
One thing is sure: We’ll never fall for this lockdown malarky again. Yay! Another prediction!
To quote Mark Twain: The glory which is built upon a lie soon becomes a most unpleasant incumbrance. … How easy it is to make people believe a lie, and how hard it is to undo that work again!
From the department of Egregious Statistics and Applied Flannel at the University of West Fantasia
The BBC published this article in which among other things they report research that shows that a person aged 85+ is 630 times more likely to die of Covid than a person aged 18-29. The arithmetic is probably correct but it’s almost completely meaningless. From the (pre-Covid) 2010-19 annual death statistics for England and Wales I have calculated that if you were a woman aged 90+ your risk of dying (of anything) was 1,346 (one thousand three hundred and forty six) times higher than that of a woman aged 20-24. Unsurprising fact: as we get older we are more likely to die. Here’s an idiotic thought: if your risk of dying from Covid is lower than your general risk in life would it lower your risk of death to catch it?
Feel free to copy/paste as much of this text and/or graphics as you would like for any reason at all. If you want to link to it I would advise making sure that the Wayback Machine (Internet Archive) has a copy so that if I change my text/graphics you can refer to what this post used to say. If you want to tear my analysis apart please do so. If you do refer to my post in any way I’d be pleased if you would let me know so that I can learn from you.
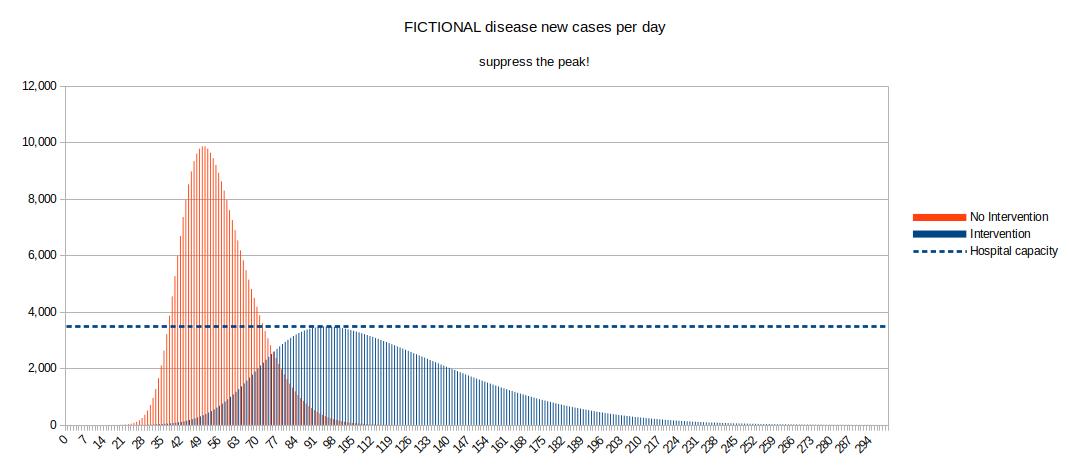
Post a comment
All comments are held for moderation; simple HTML formatting accepted.
Send feedback by e-mail , alternatively complete the form below.